This is an automatically translated article.
Posted by Master, Doctor Mai Vien Phuong - Department of Examination & Internal Medicine - Vinmec Central Park International General Hospital
Covid-19 may offer an opportunity to refine risk stratification models and help clinicians personalize screening for colorectal cancer.
1.Risk stratification for colorectal cancer screening
A personalized approach to colorectal cancer screening can help focus resources on those most at risk. Studies have shown known risk factors for colorectal cancer such as age, male sex, family history of colorectal cancer, obesity, diabetes, red meat consumption and processed meat, smoking and drinking too much alcohol. However, this method has difficulties in establishing a model that accurately identifies high-risk colorectal cancer patients.
2.Risk factors in colorectal cancer screening
Risk factors to consider for a risk stratification model of colorectal cancer based on recent studies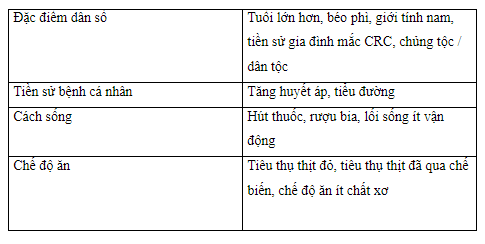
3.Studies on colorectal cancer screening stratification
A recent study using data from two international organizations of 9748 colorectal cancer cases and 10590 controls between 1992 and 2005 tested more individualized screening, incorporating environmental factors (E score) and genetics based on single nucleotide polymorphisms associated with colorectal cancer (G score). Scores are more accurate at determining colorectal cancer risk than family history. These results may encourage clinicians to recommend stronger screening for high-risk patients while creating reluctance to strongly screen those with lower scores; however, more research is still needed.
The risk of advanced cancer is even significantly increased in patients who are positive for fecal immunochemical tests. This scoring system can be used to determine which screening tool to use. Colonoscopy may be recommended for high-risk clinical patients while stool immunohistochemistry may be used initially for lower-risk patients. Instead of using stool immunohistochemistry as a negative and positive dipole value, studies show that measuring stool hemoglobin (f-Hb) levels is also useful for detecting colorectal cancer. . A retrospective analysis of 3733 asymptomatic patients over 50 years of age in Korea demonstrated that the scoring models combine f-Hb levels and clinical risk factors (age, smoking status, and clinical risk factors). diabetes) is more effective than fecal immunochemical test results.
4. Stratification of colorectal cancer screening during the Covid-19 epidemic
COVID-19 may offer an opportunity to refine risk stratification models and help clinicians personalize screening for colorectal cancer.
Studying risk factors such as those listed in Table 2 can help pave the way towards a validated risk score that is widely applicable to the general population. Further investigation of colorectal cancer-associated single-nucleotide polymorphisms may further personalize colorectal cancer risk assessment. Risk assessment may be combined with f-Hb levels based on fecal immunohistochemistry to help identify those most at risk for colorectal cancer. This personalized model will be especially important to ensure that the most at-risk patients are screened appropriately amid this global pandemic.

5. Open appointment colonoscopy (OAC)
Open appointment colonoscopy (OAC) is a service that allows patients to schedule a colonoscopy without pre-procedural evaluation by a gastroenterologist. To provide this service, a healthcare center needs to have an infrastructure in place where patients can directly schedule a colonoscopy without consulting a gastroenterologist. The hospital system coordinates open appointment colonoscopy through a variety of systems such as patient navigators or primary care physicians who manage referrals and pre-procedure procedures. Open appointment colonoscopy appears to be a possible solution to the delay in colonoscopy screening, as they show promise in increasing screening, reducing health care costs and navigating the reallocation of gastrointestinal services in the setting of COVID-19. Studies show that open access providers are booking screening colonoscopy appointments with the same effectiveness as gastroenterologists, with both health care professionals booking routine colonoscopy appointments. appropriately controlled more than 90% of the time. Patients undergoing open-appointment colonoscopy compared with patients pre-procedurally evaluated by a gastroenterologist (Open-appointment colonoscopy) had preprocedural and clinical outcomes the same.
Although the COVID-19 pandemic has caused major disruption to colorectal cancer screening, this disruption could lead to several changes in favor of current screening strategies. There may be a shift from current colorectal cancer screening and surveillance practices to developing an individualized approach based on risk factors. This will enable the allocation of resources to those at high risk and prevent inappropriate use of health care resources for those at low risk. Screening methods may also shift from direct visual methods to stool-based screening methods, such as stool immunohistochemistry. Fecal-based examination is relatively cheaper than colonoscopy while also being less invasive.
Vinmec International General Hospital is one of the hospitals that not only ensures professional quality with a team of leading medical doctors, modern equipment and technology, but also stands out for its examination and consultation services. comprehensive and professional medical consultation and treatment; civilized, polite, safe and sterile medical examination and treatment space.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.