This is an automatically translated article.
Post by Master, Doctor Mai Vien Phuong - Head of Department of Gastrointestinal Endoscopy - Department of Medical Examination & Internal Medicine - Vinmec Central Park International General Hospital
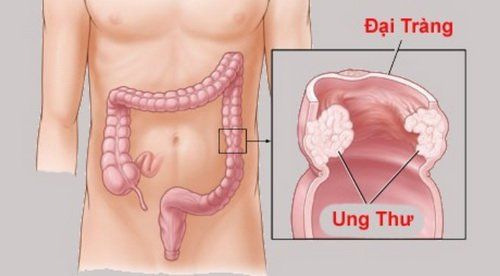
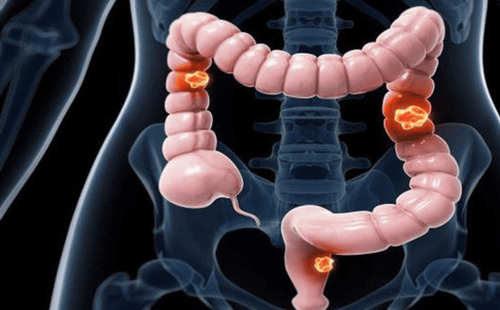
Colon cancer is a dangerous disease and has a low survival prognosis. However, if the disease is screened and detected early, there is a better chance of being treated. Therefore, the American Gastroenterology Association has offered some opinions on the age at which colorectal cancer screening should be performed.
1. Overview
Most colorectal cancers develop through adenocarcinoma sequencing, which offers an opportunity to prevent cancer by eliminating its precursor lesions. In addition to identifying colorectal cancer in its earliest stages, it is curable. Approximately 70% of sporadic colorectal cancers develop from adenomatous polyps and 25%–30% arise from sessile serrated lesions (SSL) via the SSL pathway to carcinoma.
Colorectal cancer screening efforts are aimed at removing adenomas, SSL, and detecting early-stage colorectal cancer. Certain screening modalities such as colonoscopy, sigmoidoscopy, virtual colonoscopy, and to a lesser extent stool-based testing, will detect advanced adenomatous polyps, while colonoscopy colon is optimal for SSL detection. Endoscopic polypectomy reduces colorectal cancer incidence and mortality from colorectal cancer. Given the new evidence regarding increased adherence to screening, newer approaches to colorectal cancer screening, and evidence supporting the effectiveness of screening, the aim of this article is to update the current guidelines. 2009 American Gastroenterological Association (ACG) colorectal cancer screening guide
2. Recommendations of the American Gastroenterology Association
The authors recommend colorectal cancer screening in people at average risk: Age 50 to 75 to reduce the incidence of adenomas, advanced colorectal cancer, and cancer mortality. colorectal mail. Strong recommendation, moderate-quality evidence The authors recommend screening for colorectal cancer in people at average risk 45 to 49 years of age to reduce the incidence of adenoma, advanced colorectal cancer development and mortality from colorectal cancer. Conditional recommendation; very low quality evidence The authors suggest that the decision to continue screening over age 75 should be individualized. Conditional recommendation; very low quality evidence The authors recommend colonoscopy and fecal occult blood testing as the primary screening modality for colorectal cancer screening. Strong recommendation; low-quality evidence The authors suggest considering the following screening tests for individuals who are unable or unwilling to undergo colonoscopy or fecal occult blood tests: sigmoidoscopy, laboratory testing Multifocal fecal DNA, computed tomography colonoscopy (virtual colonoscopy) or capsule endoscopy. Conditional recommendation; very low quality evidence The authors recommend against Septin 9 for colorectal cancer screening. Conditional recommendation, very low quality of evidence

3. Screening for colorectal cancer in people at average risk starting at age 45
Recent studies have highlighted the increasing incidence of colorectal cancer among people under the age of 50 in the United States. Although the incidence of colorectal cancer continues to decline in people 50 years of age and older, incidence has doubled in those aged 20 to 49 years. In 2018, the American Cancer Society published guidelines with eligibility recommendations to reduce the age to begin colorectal cancer screening from 50 to 45 years in the average-risk adult population, although the current USPSTF recommendations are to initiate screening at age 50.
These eligibility recommendations are based on analyzes of predictive modeling and epidemiological evidence age-group study of a 51% relative increase in the incidence of colorectal cancer among people under 50 years of age from 1974 to 2013. The modeling study used 2 of 3 models of the Surveillance Network and Cancer Interventions show that starting screening at age 45 is on the efficacy spectrum, and that starting screening at age 45 instead of age 50 will add about 25 years to life expectancy - the number of years achieved per 1,000 individuals. screening.
4. An alarming trend reversal in colorectal cancer incidence
Notably, in the United States the incidence of colorectal cancer in people aged 50–64 years, which had previously decreased by 2%–3% per year, increased by 1% annually from 2011 to 2016. A similar increased incidence was also observed in persons younger than 50 years of age and is attributed in part to a cohort effect at birth. The increased risk of colorectal cancer in people born after 1950 continued as they got older. It is estimated that people born around 1990 have twice the risk of colon cancer and four times the risk of rectal cancer compared with those born around the year. Although the reasons for these observations are complex and multifactorial, the fact that other developed countries are reporting similar increases in early-onset colorectal cancer and the cohort effect for found that Western lifestyles (especially exemplified by the obesity epidemic) were a significant contributor.

5. Advantages of starting screening at age 45 instead of age 50
Advantages of starting screening at age 45 instead of age 50 include a reduced risk of colorectal cancer due to early detection of colorectal cancer in this age group. Over time, detecting and removing polyps in people aged 45–49 years will reduce the incidence of colorectal cancer in people 50 years of age and older. In addition, preventing young colorectal cancer is a desirable goal because the societal impact of colorectal cancer mortality at an early age is particularly severe.
6. Disadvantages of this screening moment
The downside of such an approach is the resources required to further screen individuals aged 45 to 49 years and reduces efforts to screen individuals 50 years of age and older. In the US, the current screening rate is close to 60% (57.9% aged 50–64 and 62.4% aged 50–75). Expanding the screened population could reduce this rate by emphasizing switching to screening 45- to 49-year-olds at the expense of effort to screen unscreened 50- to 75-year-olds. A recent Markov analysis assessed the population-level impact of reducing the age of screening to 45 years and found that although starting younger can be cost-effective. However, raising screening rates in people 50–75 to the 80% goal would prevent 3 times as many deaths from colorectal cancer at about 66% less cost.
There are limited empirical data on the effectiveness of screening in younger average-risk individuals and the most appropriate screening modality in this age group is not known.
7. Checking for colorectal cancer in the elderly
With an increase in life expectancy and an increase in the geriatric population, screening for colorectal cancer in the elderly has significant public health consequences. Because several detailed subgroup analyzes of screening trials have been reported, very little empirical data exist on the best time to discontinue screening. There are a number of reasons why older adults may not receive the same benefits or may even be harmed by screening. The first reason is the reduced lifespan.
Vinmec International General Hospital is implementing a Package of Screening and Early Detection of Colorectal Cancer, implemented by a team of experienced doctors and nurses in the field of colorectal cancer diagnosis and treatment. colon, with the support of a system of modern technological equipment and facilities, full of specialized means to diagnose the disease and stage it before treatment such as: Endoscopy, CT scan, PET-CT scan, MRI, mammogram, histopathological diagnosis, gene-cell testing, ... help detect colon cancer early even when there are no symptoms.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
References
Shaukat, Aasma MD et al. ACG Clinical Guidelines: Screening for Colorectal Cancer 2021. American Journal of Gastroenterology: March 2021 - Volume 116 - Issue 3 - pp. 458-479