This is an automatically translated article.
Nosocomial infections are infections acquired during the patient's treatment at the hospital without any symptoms or during the incubation period upon admission. In some cases, the combination of antibiotics in the treatment of bacterial infections is necessary to prevent complications and poor prognosis for patients.
1. Causes and objects of risk
Nosocomial infection is a dangerous condition that occurs not only in patients but also in healthcare workers and caregivers. Therefore, it is very important to implement infection control measures to prevent and focus on treating infections (when acquired).
1.1. For patients There are many factors that lead to hospital-acquired infections in patients:
Endogenous factors: are factors originating from the patient himself such as: chronic diseases, diseases that weaken the immune system epidemics, premature infants, the elderly, people who take antibiotics for a long time... Exogenous factors: environment, air, water, waste, medical equipment, beds, procedures invasive... 1.2. For medical staff Health workers are susceptible to nosocomial infections in case of occupational accidents, exposure to blood-borne pathogens during patient care. For example:
Touching contaminated needles or sharp objects. During the procedure, blood or fluid is splashed from the patient into the mucous membranes of the eyes, nose, mouth.... Contact with blood or biological fluids containing pathogens through the skin of unhealed hands.

Nhân viên y tế cần thực hiện đúng quy trình kỹ thuật trong y tế
2. Common nosocomial infections
Nosocomial infections are often associated with the intensive care unit, of which the most common are lung infections, sepsis, then urinary tract infections and surgical site infections.
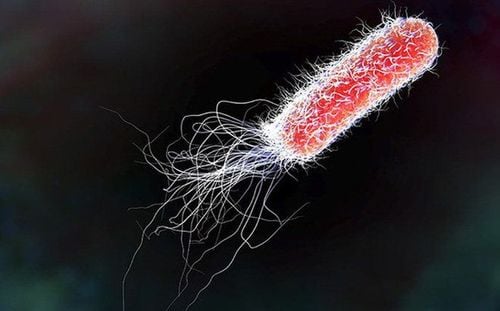
Nosocomial pneumonia: is a nosocomial infection with an incidence rate of 15-20%. Causes of pneumonia are very diverse, can be caused by viruses, bacteria, fungi... Surgical site infection: is a nosocomial infection with a high incidence only after respiratory tract infections. The cause is usually due to exogenous factors such as air, medical instruments, surgeons or medical staff. Or endogenous factors such as bacteria on the skin, at the surgical site or, rarely, blood transfused during surgery. Infection of the burn: burn patients often have sensitive skin surfaces that are easily damaged, combined with invasive interactions during treatment, are very susceptible to nosocomial infections, Staphylococcus aureus and Pseudomonas. Urinary tract infections: usually caused by Gram-negative bacilli (such as Escherichia coli, Klebsiella spp, Proteus mirabilis and P.aeruginosa, but also Enterococci and Enterobacter spp) or Candida fungi. Other types of hospital-acquired infections: sepsis, stomach and intestinal infections, eye and conjunctival infections, endometritis, etc. Hospital-acquired infections often increase morbidity and mortality. mortality, prolonging treatment time and cost of treatment, causing many difficulties for both doctors, patients and family members.
3. Note the combination of antibiotics in the treatment of bacterial infections
In most surgeries, 1 antibiotic is enough to prevent surgical site infection. Combination therapy is only recommended for patients with pre-existing signs of infection.
Note when choosing empiric antibiotics to treat bacterial infections:
Orient the type of bacteria according to the infection site. Broad spectrum antibiotics cover pathogens. The antibiotic penetrates well into the infected tissue. Some sites such as cerebrospinal fluid, prostate gland, skeletal muscle... may be difficult to penetrate, so consider choosing an appropriate antibiotic dosage form, systemic or local effect for the patient. Suitable for each patient: children, the elderly, pregnant women, people with allergies, people with impaired liver and kidney function...

Bác sĩ là người quyết định việc phối hợp kháng sinh điều trị nhiễm khuẩn
Same group of effects (same bacteriostatic or bactericidal). No effect or toxicity on the same organ. Does not stimulate bacterial resistance. Refer to the cases of antibiotic combinations that have been effective in clinical practice. Combination antibiotics are often recommended for severe infections such as:
Patients with P. aeruginosa infection with respiratory failure and septic shock. Septic shock caused by S. Pneumoniae . Febrile leukopenia, severe bacteremia. Patients with difficult to treat, multidrug resistant (MDR) agents such as Acinetobacter Spp and Pseudomonas Spp. After 48-72 hours, the doctor will evaluate the effectiveness of the combination antibiotic regimen and monitor the symptoms to make a decision to stop or continue to maintain antibiotics. Overall, the combination of antibiotics in the treatment of bacterial infections is a complex process and requires a lot of medical knowledge combined with clinical experience. To avoid unnecessary risks and complications, patients and their families should not arbitrarily combine and use different antibiotics to treat bacterial infections without the appointment or guidance from a specialist. .
If you have ever been exposed to the risk of infectious disease, you should go to the hospital to be checked by a doctor and have timely intervention.
Currently, Vinmec International General Hospital has developed a general health checkup package to help check for potential medical problems in the body. The examination is always carried out according to a process, by a team of qualified doctors with modern machinery and equipment. Therefore, customers can be assured of the quality of examination and treatment when having health problems.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.