This is an automatically translated article.
The article was consulted with Dr. Nguyen Van Duong - Interventional Cardiologist - Cardiovascular Center - Vinmec Central Park International General Hospital.Deep vein thrombosis is a common disease in severe patients, after major surgery or immobilization for many days, it can cause local symptoms or migrate to the lungs causing pulmonary embolism. Therefore, prevention of deep vein thrombosis of the lower extremities is recommended in those with risk factors.
1. What is Deep Vein Thrombosis?
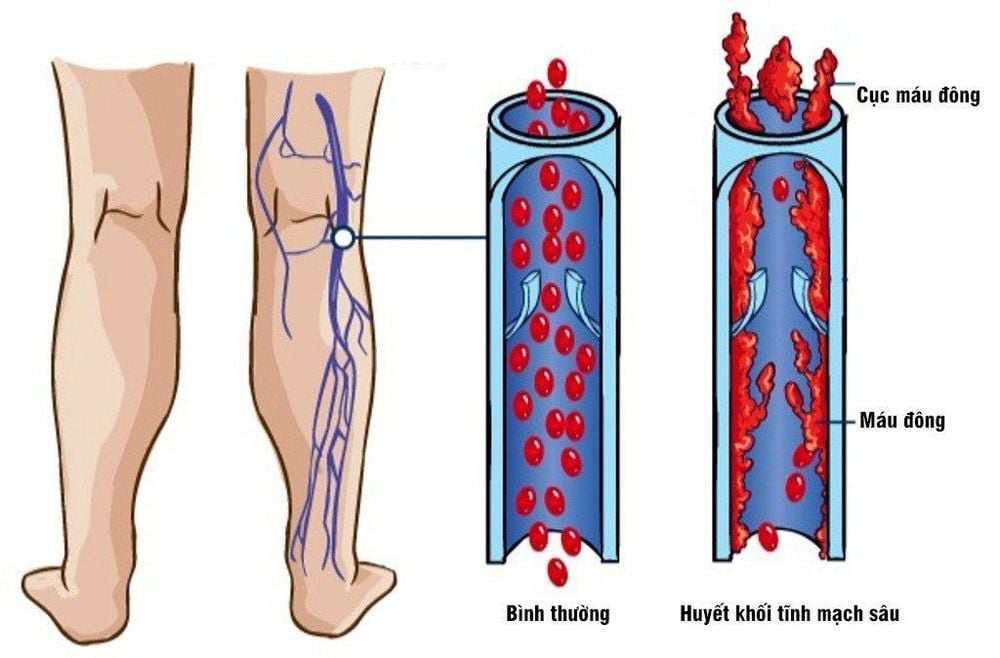
Deep vein thrombosis is a blood clot that forms deep in a vein, usually in the legs. If a deep vein thrombosis forms in the lower extremities, it is called a deep vein thrombosis of the lower extremities. Thrombosis can partially or completely block the flow of blood back to the heart and damage the one-way valves in the veins. The thrombus can also break off and travel to other organs, such as the lungs, causing a pulmonary embolism – a potentially fatal condition.2. Pathophysiology of deep vein thrombosis
The pathology of deep vein thrombosis of the lower extremities is often the result of 3 additive factors, including:Impaired venous return (eg, in immobilized patients). Endothelial damage or dysfunction (eg, after a leg fracture). Blood clotting condition. Deep vein thrombosis of the upper extremities is often the result of endothelial damage from central venous lines, pacemakers, or injection drug use. Deep vein thrombosis of the upper extremities sometimes occurs as part of superior vena cava syndrome (SVC) (compression or invasion of the superior vena cava by a tumor and causes symptoms such as facial swelling and varicose veins). neck veins and facial flushing) or due to hypercoagulability or compression of the subclavian veins.
Deep vein thrombosis consists of thrombin, fibrin, and red blood cells with relatively few platelets (red thrombus). Without treatment, the thrombus can spread to the proximal segment or migrate to the lungs.
3. Risk factors for formation of deep vein thrombosis of the lower extremities
Many risk factors can contribute to the formation of DVT, including:Age over 60. Cancer is a risk factor for DVT, especially in older patients. and patients with recurrent thrombosis. The association was strongest for mucinous epithelial cell cancers such as bowel or pancreatic cancer. Smoking (both active and passive smoking). Use of estrogen receptor-stimulating agents (eg, tamoxifen, raloxifene), estrogen supplement therapy. Heart failure, nephrotic syndrome, myeloproliferative disease. Hypercoagulable diseases: Antiphospholipid syndrome, antithrombin deficiency, factor V Leiden mutation (activation of protein C resistance), heparin-induced thrombocytopenia, increased factor VIII, increased factor XI, decreased protein C, decreased protein S, paroxysmal nocturnal hemoglobinuria. Immobilization, trauma, obesity, pregnancy. Surgery within 3 months.
4. Methods to prevent deep vein thrombosis of the lower extremities
Prophylaxis of DVT in the lower extremities is better and safer than treatment when a thrombus has already formed, especially in high-risk patients. Therefore, the risk of deep vein thrombosis should be assessed and treatment considered according to the following steps.Step 1: Assess the risk of developing deep vein thrombosis Low-risk patients (undergoing minor surgery but no DVT risk factors; those temporarily inactive for a while long periods of time, such as a flight of >6 hours) should be encouraged to walk or move the legs periodically, flexing the instep 10 times/hour is probably sufficient; no need for medical treatment. Patients at higher risk include those undergoing minor surgery but have risk factors for deep vein thrombosis; those undergoing major surgery, especially orthopedic surgery, even in the absence of risk factors, and bedridden patients with serious medical conditions (eg, care unit patients). active, patients with heart failure, chronic obstructive pulmonary disease, chronic liver disease, stroke). These patients require prophylactic treatment. In addition, the PADUA score can be used to assess the risk of VTE. If PADUA is less than 4, the risk is low. If PADUA ≥ 4 points is high risk. Step 2: Assess contraindications, bleeding risk of anticoagulation according to the IMPROVE scale Evaluate contraindications based on medical conditions such as liver failure, renal failure, bleeding (brain, gastrointestinal) , blood clotting disorders, platelet count, current anticoagulants, surgical procedures,... If the IMPROVE score has a total score of ≥ 7, the risk of bleeding is high, or bleeding is clinically significant. . Step 3: Weigh the benefits and risks of anticoagulation for each patient. If there are contraindications or high bleeding risk score (IMPROVE ≥ 7), do not use anticoagulation. Mechanical methods should be selected for prevention. If anticoagulation is not contraindicated and there is an IMPROVE bleeding risk score <7, anticoagulation should be used. Step 4: Select the appropriate method and duration of prophylaxis There are many ways to prevent deep vein thrombosis of the lower extremities, the choice depends on the patient's risk level, type of surgery, and duration of prophylaxis. , contraindications, side effects, cost, ease of use.
Mechanical therapy (eg: Compression device or compression stockings, venipuncture) After surgery, it is necessary to elevate the leg and avoid prolonged immobility. The benefit of compression stockings is unclear in low-risk surgical and medical patients. However, combining compression stockings with other preventive measures may be better than each measure alone.
Intermittent pressure (IPC) inflatables use a pump to periodically inflate and deflate, providing external compression to the legs and thighs. After surgery, IPC may be used in place of or in combination with anticoagulants. IPC is recommended for surgical patients at high bleeding risk and with contraindications to anticoagulation. IPC is probably more effective in preventing calf thrombosis than proximal thrombosis. IPC is contraindicated in some patients who are obese or have lower extremity artery disease. For patients at increased risk for DVT and very high bleeding risk (eg, after major trauma), IPC is recommended until bleeding risk is reduced and injections can be made. anti freeze blood.
Inferior vena cava filters do not prevent lower extremity DVT from forming but are sometimes used to prevent pulmonary embolism in patients with contraindications to anticoagulation or recurrent DVT. despite adequate anticoagulation. The use of vena cava filters should be avoided unless thrombosis has been confirmed.
Drug therapy (including low-dose unfractionated heparin, low-molecular-weight heparin, warfarin, fondaparinux, oral direct anticoagulants). Low-dose unfractionated heparin (UFH) 5000 units is given subcutaneously 2 hours before surgery and every 12 hours. Bedridden patients who did not undergo surgery received 5000 units subcutaneously every 12 hours until risk factors were reversed.
Low molecular weight heparins (LMWHs) are more effective than low-dose UFH in the prevention of lower extremity deep vein thrombosis and PE. Enoxaparin 40 mg subcutaneously once daily, dalteparin 5000 units subcutaneously once daily, and tinzaparin 4500 units subcutaneously once daily appear to be equally effective. Fondaparinux 2.5 mg subcutaneously daily is at least as effective as LMWH in patients undergoing orthopedic surgery and may be more effective than LMWH after orthopedic surgery.
Warfarin, using a target international normalized ratio (INR) of 2.0 to 3.0, has been shown to be effective in orthopedic surgery but is being gradually replaced by LMWHs and anticoagulants. drink new generation because easier to use.
Oral direct anticoagulants (eg, dabigatran, rivaroxaban, apixaban) are as effective and safe as LMWH for the prevention of lower extremity deep vein thrombosis and PE following hip or knee replacement surgery.

Please follow the website: Vinmec.com regularly to update many other useful information.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
Reference articles: msdmanuals.com, vnha.org.vn, timmachhoc.vn













