This is an automatically translated article.
The article was professionally consulted by Specialist Doctor I Huynh Kim Long - Emergency Resuscitation Doctor - Emergency Resuscitation Department - Vinmec Da Nang International General Hospital. Dr. Huynh Kim Long has extensive experience in the treatment of Resuscitation - Emergency and Acute Stroke in adults.Multi-organ failure syndrome is defined as when organ function is altered in critically ill patients and the homeostasis cannot be compensated for. This condition is often critical, affects the in-hospital prognosis, and requires comprehensive care in the intensive care unit, especially prompt correction of shock from any cause.
1. What is multi-organ failure syndrome due to prolonged shock?
Shock is defined as hypoxia in cells and tissues due to decreased oxygen supply, increased oxygen consumption, inadequate oxygen utilization, or a combination of these processes. This is a consequence of circulatory failure, which manifests as hypotension , that is, with tissue hypoperfusion. However, it is important to recognize that a patient in shock may still have an initial presentation of hypertension or normal blood pressure but the oxygen supply has become inadequate to meet the metabolic needs of the patient. cell metabolism.In clinical practice, shock is approached according to classification, main pathophysiology, or clinical presentation. In particular, the shock classification is the most useful method, because it both suggests the cause and pathophysiology of the underlying disorder, and helps guide the treatment of the patient out of shock and restore metabolism. of cells. Shock is classified into 4 main groups: hypovolemic shock (acute blood loss, acute diarrhea...), cardiogenic shock (myocardial infarction, arrhythmia...), Shock due to extracardiac obstruction (pulmonary, aortic occlusion..), Distributive shock (septic shock, neurogenic shock...)
Although the effects of initial shock are reversible, if this cannot be reversed quickly, prolonged shock leads to multiple organ failure and increased risk of death. Specifically, multi-organ failure, also known as multi-organ dysfunction syndrome, is a state of dysfunction of the body's organ systems with clinical and biochemical evidence following an injury or Acute illness and prolonged shock are also a cause.
The onset of this complication usually occurs on one organ system, but if the body cannot quickly compensate, other organ systems will also be successively affected. As a result, multiple organ failure contributes to about 50% of deaths in the ICU. However, with timely and correct positive adjustments, the patient can improve completely without leaving any sequelae.

2. What are the possible causes of multi-organ failure syndrome due to prolonged shock?
Almost any reason that drives a patient into shock can lead to complications of multiple organ failure :Sepsis Major trauma Large area burns Acute pancreatitis Acute blood loss Repeated blood transfusions Myocardial infarction Acute heart failure Autoimmune disease Heat illness Eclampsia Poisoning, drug overdose.
3. How to approach multi-organ failure syndrome due to prolonged shock?
Multi-organ failure syndrome is a serious condition, with systemic manifestations, so it should be approached in the etiological syndromes that cause shock and lead to this complication. Therefore, the clinician when approaching multi-organ failure syndrome due to prolonged shock should recognize the following conditions:Presence of systemic inflammatory response and dysfunction of at least two organ systems with levels that can be mild or severe or can lead to death. Organ system dysfunction is manifested by: Acute kidney injury and blood-metabolic acidosis Respiratory critical syndromes (ARDS) Cardiomyopathy Encephalopathy Gastrointestinal dysfunction with Symptoms of: Increased intestinal wall permeability due to bacterial toxins and endotoxins, decreased intestinal motility, acute pancreatitis, stress ulceration of the gastrointestinal mucosa, reactive cholecystitis, ischemia at bowel or intestinal infarction. Hepatic dysfunction Coagulation disorders and bone marrow suppression of blood cell lines.

4. How to treat multi-organ failure syndrome due to prolonged shock?
When a patient is in shock for which the cause cannot be distinguished, it is important that the clinician immediately initiate therapy while identifying the cause so that the patient can be rescued from this critical condition. . In particular, early recognition is the key to successful treatment.Patients who are found to have signs of shock and multiple organ failure will require intensive care in the critical care unit with cause-specific therapies and comprehensive support, including:
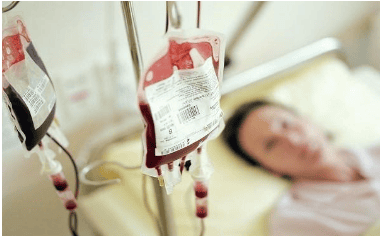
Antibiotic therapy for septic shock or as soon as superinfection is suspected to control early foci of inflammation. Surgical intervention such as isolation, drainage, rinsing if indicated. Fluid resuscitation is intended to ensure effective circulating volume in hypovolemic shock. If the patient has an acute blood loss with a large amount, it is necessary to replace whole blood or red blood cells. However, if suitable blood products are not available, crystalloids or macromolecular solutions should be substituted. Prescribe vasopressor drugs, inotropic drugs early if anaphylaxis, distributive shock or cardiogenic shock is suspected. However, the effectiveness of this therapy is only achieved when the lumen volume is guaranteed. Therefore, it is necessary to ensure an effective volume of circulating fluid through the parameters of vital signs, balance water in and out, and avoid fluid overload. Support organ function with medical equipment such as ventilator, aortic balloon counterpulsation, continuous dialysis or extracorporeal circulation. Control blood glucose levels, maintain within a safe range of 6 to 10 mmol/L. Ensure adequate energy and balanced nutritional sources. The best route of feeding is encouraged through the gastrointestinal tract. Seek and treat the underlying cause, comorbidities, and complications caused by shock or multiple organ failure.

5. What is the prognosis of multi-organ failure syndrome due to prolonged shock?
Once the patient has fallen into a state of prolonged shock leading to multi-organ failure syndrome, the prognosis is often quite severe. Prolonged shock may result from failure of early recognition or failure of immediate medical interventions, progressive tissue hypoxia, and eventual organ failure.Statistics show that the mortality rate in patients with prolonged shock and complications of multiple organ failure is up to 60 to 98%. Among them, circulatory collapse is often the last critical factor. If they survive, about 50% of people with multiple organ failure will find it difficult to return to work or normal activities after 1 year of follow-up. However, there are always many cases where there is a chance for a complete recovery if treated to escape shock and support the function of organ systems.
In summary, prolonged shock that can lead to multi-organ failure syndrome is a frightening complication for patients in the ICU. This is also a warning for doctors when approaching patients as soon as there are signs of shock. Only with early detection and timely correction can the patient's prognosis become better.
Vinmec International General Hospital with a system of modern facilities, medical equipment and a team of experts and doctors with many years of experience in medical examination and treatment, patients can rest assured to visit. examination and treatment at the Hospital.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.














