This is an automatically translated article.
Posted by Master, Doctor Mai Vien Phuong - Department of Examination & Internal Medicine - Vinmec Central Park International General Hospital
Abbreviations
Inflammatory bowel disease (IBD)
Ulcerative colitis (UC)
The exact roles of thiopurines, azathioprine and 6-mercaptopurine in ulcerative colitis (UC) regimens have been debated. In particular, their use in UC remains controversial because the evidence lies in small clinical trials. In this article, we briefly review the evidence on the therapeutic efficacy of thiopurine.
Medical treatment of ulcerative colitis can be complex, and it is often stratified based on the extent of the disease. The goal of treatment is remission, followed by a maintenance regimen for continued clinical and endoscopic remission. The exact roles of thiopurine, azathioprine and 6-mercaptopurine, in UC treatment algorithms have been debated. In particular, their use in UC remains controversial, as the evidence lies in small clinical trials.
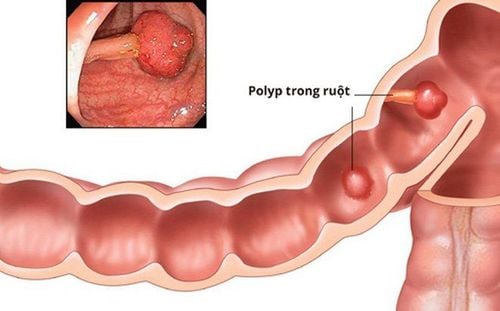
1. Overview of Ulcerative Colitis
The prevalence of ulcerative colitis (UC) is increasing globally. Furthermore, UC leads to a significant economic burden; Total direct costs attributable to UC in the United States are estimated at $3.4-8.6 billion annually, and about 50% of patient costs are incurred as a result of hospitalization.
Although some UC patients eventually require colectomy, many can be managed medically with medical therapy. Medical treatment for UC can be stratified based on the severity of the disease; 5-aminosalicylates such as sulfasalazine, mesalamine, and balsalazide form the basis of therapy for mild to moderate disease, followed by immunomodulators and finally anti-tumor necrosis alpha (anti-TNF) drugs.
In recent years, there has been considerable debate about the place of the drugs thiopurine, azathioprine and mercaptopurine, in induction and maintenance treatment algorithms for UC.
2. History of Thiopurine use in the treatment of ulcerative colitis
The use of azathioprine for UC was first reported in 1966. Azathioprine is a drug that is converted to 6-mercaptopurine (6-MP). Xanthine oxidase, thiopurine methyltransferase (TPMT), and hypoxanthine phosphoribosyl transferase then convert 6-MP to 6-thiouric acid, 6 methylmercaptopurine (6-MMP), and precursors of the corresponding active 6-thioguanine nucleotides (6-TGN) response. 6-TGN is incorporated into nucleic acids and ultimately inhibits the synthesis of proteins, ribonucleic acid (RNA), and deoxyribonucleic acid (DNA); however, the mechanism of action of azathioprine has not been fully explored.
TPMT activity levels are checked regularly before starting azathioprine, as TPMT-deficient patients are at increased risk for severe myelosuppression. For people with normal TPMT levels, the dose of azathioprine is usually 2-2.5 mg/kg body weight/day. In addition to the risk of myelosuppression, azathioprine and 6-MP carry a risk of characteristic reactions such as fever, pancreatitis, rash, and arthralgia. Hepatotoxicity from azathioprine and 6-MP is particularly associated with 6-MMP levels. Although hepatotoxicity can sometimes be seen with low concentrations of 6-MMP, the risk is 3-fold increased with high concentrations of 6-MMP (levels > 5700 pmol/8 x 10 red blood cells).
3. Efficacy of azathioprine in the treatment of ulcerative colitis
Regarding its effectiveness as an inducer, azathioprine has had mixed results in UC. Ardizzone and colleagues investigated the efficacy of azathioprine versus mesalamine in achieving corticosteroid-free remission (as defined both clinically and endoscopically) in steroid-dependent UC, and found azathioprine to have more effective.
Author Sood and colleagues studied the efficacy of azathioprine plus sulfasalazine and corticosteroids compared with the latter two drugs alone in providing remission in severe UC, and found no significant difference in the rates of disease. remission rates between the two groups. 6 In 1990, Steinhart, et al. Retrospective review results of initiating azathioprine therapy in a small cohort of UC patients receiving in-clinic corticosteroids. The efficacy of azathioprine was defined as the ability to reduce prednisone to less than 50% of the pre-treatment dose without relapse and improve clinical symptoms. Most patients (12 out of 16) responded to azathioprine, and the authors concluded that azathioprine was beneficial for patients with corticosteroid-resistant or dependent UC.

4. Efficacy of azathioprine in maintaining remission in steroid-dependent UC
Studies on the effectiveness of azathioprine in maintaining remission in steroid-dependent UC have also shown mixed results. Sood and colleagues performed a study in 2002 evaluating azathioprine and sulfasalazine or sulfasalazine and placebo in 35 patients with severe UC; All patients were initially treated with corticosteroids. Fewer patients in the azathioprine and sulfasalazine groups experienced a UC recurrence compared with the sulfasalazine and placebo-treated groups, and this difference was statistically significant.
On the other hand, Sood and colleagues in another study found no significant difference in remission rates among UC patients on maintenance therapy with azathioprine or sulfasalazine. However, this study was quite small (n = 25). Previous studies also showed no significant difference between azathioprine and placebo in remission rates; for example, Jewell and Truelove showed no difference in 12-month remission rates (determined by endoscopic detection of inflammation or bright red blood per rectum) when azathioprine was compared with placebo.
5. Role of azathioprine in maintaining UC remission in severe or steroid-dependent cases
Due to conflicting reports in smaller studies, several groups have attempted to address the efficacy of azathioprine in UC using a synthetic approach. In the systematic review by Leung et al., 5 studies were analyzed to evaluate the effectiveness of azathioprine in maintaining UC remission in severe or steroid-dependent cases. Four of the five studies used 2-2.5 mg/kg b.w./day of azathioprine, and there was significant heterogeneity between these studies. Their meta-analysis showed a mild efficacy of azathioprine in maintaining clinical remission of UC (hazard ratio [RR], 1.42); however, this was not statistically significant (95% confidence interval [CI], 0.93-2.17; p = 0.109).
The studies used in the meta-analysis were limited by small sample sizes (between 25-80 participants), significant heterogeneity, and the use of specific analyses, such as risks. relative risk in the random-effects model versus the fixed-effects model and the pooled relative risk estimate.
6. Some other studies on the role of azathioprine
Another meta-analysis in 2009 aimed to clarify these issues in patients with severe UC or steroid dependence. Four studies, with a total of 89 patients, were analyzed to evaluate the effectiveness of azathioprine/6-MP compared with 5-ASA or placebo in inducing UC remission. This comparison did not show a significant difference between the two groups (OR, 1.59; 95% CI, 0.59-4.29.
In addition, six studies with a total of 124 patients were used for this study. compared azathioprine/6-MP with 5-ASA or placebo to maintain UC remission; statistically significant differences were found between the two groups (OR, 2.56; 95% CI, 1.51- 4.34) Gisbert and colleagues further subdivided this part of the analysis to compare azathioprine/6-MP vs placebo and then azathioprine/6-MP vs 5-ASA; prior meta-analysis This was statistically significant, in favor of azathioprine/6-MP in maintaining UC remission, whereas the latter analysis failed to achieve a statistically significant difference in efficacy. Synthesis of the efficacy of azathioprine/6-MP in maintaining UC remission is difficult to interpret.
A systematic and meta-analysis by Khan and colleagues, using inclusion criteria More rigorous research, aimed at researching an up-to-date literature base on the efficacy of azathioprine in inducing UC remission and preventing relapse. There are 2 randomized controlled trials that have investigated the efficacy of azathioprine in inducing remission in active UC. They found a trend toward the benefit of azathioprine over placebo; however, this was not statistically significant (RR, 0.85; 95% CI, 0.71-1.01; p = 0.67). There was no statistically significant heterogeneity between the two studies; however, both studies were small (n = 20-25).
In three RCTs that investigated the use of azathioprine in maintaining remission, there was a statistically significant benefit of azathioprine over placebo in preventing relapse. Again, however, the studies included were small. Notably, the studies analyzed in this meta-analysis were similar to those studied in Leung, et al. synthetic analysis. While Leung and colleagues jointly analyzed all trials, Khan, et al.

7. Is azathioprine alone effective in treating patients with moderate to severe UC?
In a comparative efficacy trial, Panaccione and colleagues recently studied 239 patients with moderate to severe UC to evaluate corticosteroid-free clinical remission in those treated with infliximab alone. toxic, azathioprine alone or in combination with infliximab and azathioprine. The study duration was 16 weeks and the dose of infliximab was 5 mg/kg at weeks 0, 2, 6, and 14, and the dose of azathioprine was 2.5 mg/kg b.w./day. A higher proportion of patients receiving combination therapy achieved corticosteroid-free remission at week 16 than azathioprine monotherapy (p = 0.032) or infliximab monotherapy (p = 0.017).
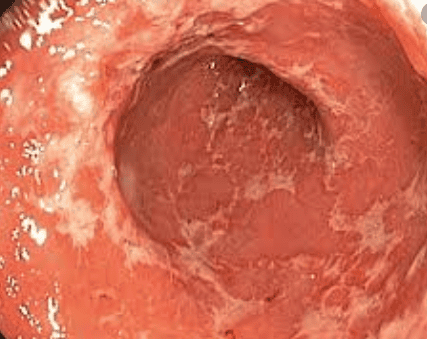
In addition, mucosal healing at 16 weeks based on a Mayo-endoscopic subscore of 0 or 1 was more likely to be seen in those treated with combination therapy than azathioprine monotherapy (p = 0.001). There was a greater improvement in the total Mayo score and the Inflammatory Bowel Disease Questionnaire (IBDQ)/Short Health Survey (SF-36) score in the combination treatment group when compared to azathioprine or monotherapy. infliximab. Therefore, this study suggests that combination therapy rather than azathioprine alone is superior in clinical and endoscopic remission of moderate to severe UC.
Conclusion
Overall, data on the effectiveness of thiopurine in UC are limited by small studies. While meta-analyses have found a trend toward the benefit of azathioprine over placebo in stimulating and maintaining remission in UC, these studies are limited by heterogeneity and method. analysis. Furthermore, there are no firm data from these studies to suggest that azathioprine monotherapy would be beneficial for the induction and maintenance of UC remission. It seems that the most important role of thiopurines in the medical treatment of UC may be as an adjunct to biologic therapy. Perhaps earlier, more aggressive therapy with biologic therapy was warranted in patients with severe or steroid-dependent UC. Thiopurine monotherapy could certainly be considered in steroid-dependent or drug-resistant patients with contraindications to biologic therapy, but this patient population appears to be small. Monotherapy with azathioprine or 6-mercaptopurine may also be considered in cases with limited access to biologic therapy.
Vinmec International General Hospital with a system of modern facilities, medical equipment and a team of experts and doctors with many years of experience in medical examination and treatment, patients can rest assured to visit examination and treatment at the Hospital.
If you have a need for consultation and examination at Vinmec Hospitals under the national health system, please book an appointment on the website for service.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
References
Molodecky NA, Soon IS, Rabi DM, et al. Increasing prevalence and prevalence of the inflammatory bowel diseases with time, based on systematic review. Gastroenterology. 2012;142:46. Marchioni Beery R, Kane S. Current approaches to the management of new-onset ulcerative colitis. Clin Exp Gastroenterol. 2014;7:111-32. Levesque BG and Loftus EV. Conventional medical management of ulcerative colitis: Azathioprine, in Baumgart, DC, Crohn's Disease and Ulcerative Colitis: From Epidemiology and Immunobiology to a Rational Diagnostic and Therapeutic Approach, Springer, New York, p. 473-480. Raina Shivashankar and Edward V. Loftus, Efficacy of Thiopurine Monotherapy in Ulcerative Colitis, Practical gastroenterology • october 2015