This is an automatically translated article.
Post by Master, Doctor Mai Vien Phuong - Department of Examination & Internal Medicine - Vinmec Central Park International General Hospital
Primary intestinal lymphadenopathy (primary lymphatic vasodilatation) was first described in 1961 by Waldmann et al. (PLE). Primary lymphatic vasodilatation is caused by diffuse or local dilation and/or rupture of intestinal lymphatic vessels in the mucosa, submucosa, or adnexa due to high pressure in the lymphatic vessels.
It is important that the prevalence and etiology remain unknown. However, genetic associations have been discussed since the diagnosis is often established in childhood with very rare cases in adults. Symptoms were largely related to the severity of the lymphatic loss and the ongoing loss of proteins leading to hypoproteinaemia, lymphopenia, and decreased serum immunoglobulin levels. Among others, these symptoms include edema of the lower extremities, generalized edema, as well as pleural, pericardial, or often abdominal effusion.
1. Clinical case
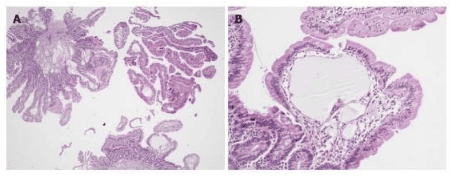
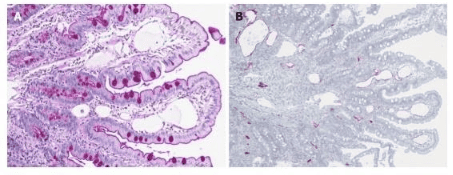
In October 2018, a 34-year-old Austrian woman presented with recurrent nausea independent of food intake, abdominal discomfort, fatigue, occasional diarrhea as well as increased susceptible to opportunistic infections i . After ending her pregnancy earlier this year, she reported more frequent swelling of her limbs. Other medical histories included comorbidities and negligible drug intake. It is worth noting that transient facial edema has occasionally been reported in childhood, starting at age 12. After puberty, markedly marked lower extremity edema, nausea, and persistent fatigue were observed. reported, but disappeared with oral contraceptive use or during pregnancy. Clinical examination at initial exposure revealed no abnormalities. Especially, there was no edema in the upper or lower limbs and the weight was stable with a body mass index of 18.3 kg/m2. Biochemical examination revealed polycythemia vera, hypoalbuminemia, transient hypoglycemia and leukopenia, immunoglobulins decreased, CD4:CD8 T-cell ratio decreased, Urine sediment was free of protein. urinary tract and no signs of kidney, liver, pancreas, or heart disease. Bone marrow analysis revealed no myeloma nor invasive lymphoma and ß2-microglobulin was within the normal range excluding hematologic disease. Computed tomography of the abdomen and pelvis showed thickening of the ileum and jejunum walls with up to 32 mm enlarged mesenteric lymph nodes localized to the lower abdomen. Therefore, ileostoscopy with exploration of >8 cm of ileum from the ileocecal valve was performed with normal results. After the CT results were confirmed on magnetic resonance imaging, gastroscopy up to D2 of the duodenum revealed white spots of the duodenal mucosa, suggesting lymphedema. However, histological evaluation did not reveal evidence of dilated lymphatic vessels or primary lymphatic vasodilation, giardiasis, celiac disease, Whipple disease, or enteropathy, which was also excluded by normal calprotectin levels. Following a video capsule endoscopy showing a snowflake appearance of the mucosa, double-balloon enteroscopy revealed approximately 70cm of a verified mucosal lesion of the jejunum compatible with lymphoid tissue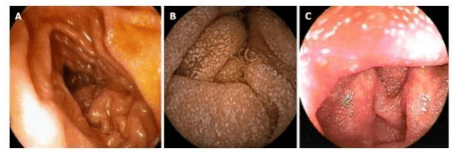
Treatment and outcome in this patient
After placing the patient on a high-protein medium-chain triglyceride (MCT) diet, the patient's clinical condition improved significantly within 4 weeks . Up to 2 years after diagnosis, mild lower extremity edema was observed only from the end of lactation to the second pregnancy, and abdominal discomfort, fatigue, and nausea improved. significantly good. Laboratory improvement was characterized by an increase in total serum protein, albumin, and quantitative immunoglobulin.
2. Prevalence of primary lymphatic vasodilatation
Because of the rarity of this disease, the worldwide prevalence of primary lymphatic vasodilatation in humans is unknown. However, genetic predisposition has been discussed as if it mainly affects children under 3 years of age. This is supported by familial forms of syndromes associated with primary lymphatic vasodilation, including yellow nail syndrome, von Recklinghausen disease, Turner, Noonan, Klippel-Trenaunay, or Hennekam syndrome. However, cases in adult patients persist. The authors performed a review of the literature and were able to identify 49 cases from 46 reported clinical cases of primary lymphatic vasodilatation in adults, where symptoms started after the age of 18 years. Notably, 27/46 (58.7%) have been published since 2010, suggesting that this entity is increasingly recognized and its popularity may be underestimated.
Median age at diagnosis
Median age at diagnosis was 43 (range: 20-83) years while the median time from symptom onset to final diagnosis was 3 (range: 0-40) years, highlighting the difficulty in accurately diagnosing this subject. Although a literature review of primary lymphatic vasodilatation has existed reporting a mean age of 13.3 years at onset of symptoms and 8.5 years at diagnosis, indicated that 75% of the cases in this review included patients with onset of symptoms before the age of 20 years. Regarding the sex distribution, 22 male cases (44.9%) and 27 female cases (55.1%) were reported.
Clinical manifestations of primary lymphatic vasodilatation
The author's case describes a 34-year-old woman who was diagnosed with primary lymphatic vasodilatation approximately 22 years after the first episode of edema and 22 weeks after the first episode. first contact. She presented with nausea, abdominal discomfort, diarrhea, and bilateral edema of the limbs. From 48 patients who reported symptoms in the literature, 40 patients (83.3%) reported the presence of any peripheral/systemic edema while only 2 patients had no edema and 6 case reports did not report this symptom. The majority (n= 27, 56.3%) reported only bilateral lower extremity edema. 9/48 patients (18.8%) presented with abdominal pain, 13 patients (27.1%) ascites (chylous), 10 patients (20.8%) pleural effusion and 4 patients (8 (8). ,3%) pericardial effusion. Diarrhea occurred in 20/48 patients (41.7%). Other rare nonspecific symptoms include weight change, nausea, general weakness, pallor, and gastrointestinal bleeding. These findings are consistent with a previous literature review of 84 cases of primary lymphatic vasodilatation (including mainly children), which reported limb edema, diarrhea, ascites, and lymphedema, respectively. are 78%, 62%, 41% and 22%. These symptoms and their varying degrees can largely be explained as a consequence of lymph/protein and subsequently dehydration due to lower vascular pressure in the interstitial fluid. Relevance of Symptoms and Hormones The fact that pregnancy and oral contraceptives led to the disappearance of edema in the author's patient is truly surprising as this has not been reported. Notably, the symptoms completely disappeared when taking oral contraceptives and reappeared in the days of not taking the pill midway. One could hypothesize that differences in estradiol might influence the severity of lymphedema: Morfoisse et al., who explored the role of estrogens in lymphatic endothelial cells , found that estradiol protected lymphedema and that the blockage of the estrogen receptor was associated with lymphatic leakage. However, this has only been shown in an animal model of secondary lymphedema and no other studies have provided further evidence of this mechanism.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
References Huber R, Semmler G, Mayr A, Offner F, Datz C. Primary inflammatory bowel disease in adult patients: Case report and literature review. World J Gastroenterol 2020; 26 (48): 7707-7718 [PMID: 33505146 DOI: 10.3748 / wjg.v26.i48.7707 ]