This is an automatically translated article.
The article was written by MSc Nguyen Quoc Tuan - Head of Internal Medicine Unit - Dialysis, Department of General Internal Medicine - Vinmec Times City International General Hospital.Normally, each person has 2 kidneys (in some special cases only one or more than 2) pea-shaped located in two lumbar fossa along both sides of the spine from the XII thoracic vertebra to the lumbar vertebrae. I - II. Each kidney is made up of about 1 million Nephrons.
1. The glomerulus and the function of the kidney
Nephron is the structural and functional unit of the Kidney. The Nephron consists of two parts: the glomerulus and the tubule. The glomerulus consists of an outer sac and an inner vascular coil. The renal tubule is a tube with many bends, one end is continuous with the glomerulus and the other end drains into the collecting duct.
One of the main functions of the kidneys is to make urine to remove water and waste products of metabolic processes in the body.
Blood is brought into the kidney with a very large flow (1200ml/min) and then to the glomerular coil, where a large amount of plasma (about 120ml/min) from the blood through the glomerular filter enters the water cavity. The glomerulus produces the first urine.
Due to the structure of the glomerular membrane, proteins (albumin) and blood cells are retained in the blood. The first urine from the glomerulus passes through the renal tubule, at the renal tubule, the first urine is reabsorbed, exchanged for ions, then passed through the collecting duct to form final urine and poured into the renal pelvis and then down the ureter to the bladder. before being discharged from the body.

2. Glomerular disease
2.1 Definitions
Processes that damage the structure and change the function of the glomerulus are called glomerular diseases. If the disease is limited to the glomeruli, it is called primary glomerulopathy.
Systemic diseases that cause damage to many organs including the kidneys, then the glomerular disease is called secondary glomerulopathy.
2.2 Expression and classification
Glomerular disease presents in a variety of ways depending on the cause of the glomerular damage. Many cases of the disease have no clinical symptoms but are detected through urinalysis during a general physical examination or to find the cause of another disease.
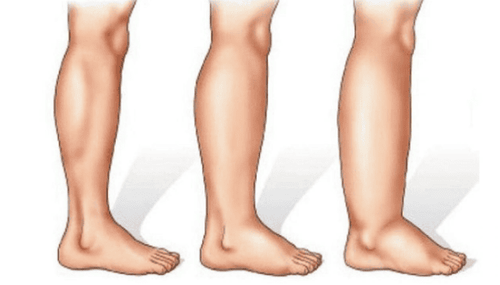
Besides asymptomatic cases, glomerulonephritis is also detected when there are clinical manifestations such as hypertension, edema, fatigue (due to renal failure, anemia).... Sometimes patients are detect glomerular damage when there are manifestations of systemic disease such as emaciation, fatigue, persistent fever, arthralgia, rash...
Clinical and laboratory symptoms of glomerulonephritis are divided into The two main types are glomerulonephritis syndrome and nephrotic syndrome, but some diseases have a mixture of both syndromes.

2.2.1 Glomerulonephritis syndrome
Patients with glomerulonephritis syndrome often show:
Urine test by test strip is positive for red blood cells, urine sediment examination shows irregular red blood cells, possibly accompanied by red blood cell casts Protein (albumin) ) in the urine with varying degrees of edema, especially anterior tibial edema, hypertension (blood pressure > 130/80 mmHg) Decreased ability of the kidneys to filter toxins, leading to an increase in blood urea and creatinine, the Severe cases may be oliguria (little urine) or anuria (no urine).
Glomerulonephritis syndrome often occurs secondary to inflammatory reactions due to immune disorders, infections, vasculitis ..... Some kidney diseases with glomerulonephritis syndrome are:
IgA nephropathy Kidney disease due to Lupus Post-infectious nephropathy (especially group A beta-hemolytic streptococci) Vasculitis (inflammation of the small vessels of many organs including the glomerular microvasculature) Cryoglobin nephropathy in the blood (with precipitation of blood proteins ) Proliferative membranous glomerulonephritis IgA nephropathy associated with vasculitis (Henoch-Schonlein pupura)
2.2.2 Nephrotic syndrome
Nephrotic syndrome is caused by a damaged glomerular membrane that does not prevent protein from escaping from the plasma into the urine, resulting in a large amount of protein loss (more than 3.5 g/24 hours) in the urine. Nephrotic syndrome manifests as:
Proteinuria a lot (over 3.5 g/24 hours). Decrease in protein (especially albumin) in the blood, increase in blood lipids. Increased blood clotting (due to loss of natural anticoagulants in the urine). Edema (due to decreased colloidal pressure due to loss of albumin in the blood). In some cases, there may be kidney failure (increased urea, blood creatinine). No or very few red blood cells, erythrocytes in the urine.
Nephrotic syndrome can be primary or secondary to systemic diseases. Some kidney diseases associated with nephrotic syndrome are:
minimal change disease focal segmental glomerulosclerosis Membranous nephropathy Diabetic nephropathy Amyloid kidney disease (formerly known as kidney powder disease)
3. Diagnosis of glomerular disease
Glomerular diseases are diagnosed based on urinalysis, blood tests, and imaging of the urinary system. However, in many cases, the definitive diagnosis of glomerulonephritis must be based on renal biopsy for histopathological examination.
Urinalysis Use test strips to detect protein and red blood cells in the urine, quantify protein to know more or less, check sediment to see irregular erythrocyte morphology and red blood cell casts.
Blood tests Quantify urea and creatinine to know kidney function (the concentration of these substances increases in the presence of kidney failure).
Test for immunological factors (Antinuclear antibody, complement, anti-glomerular basement membrane antibody, ANCA ....), blood sugar test, ASLO, protein electrophoresis in serum as well as in urine .... helpful in identifying the general pathology causing secondary glomerular injury.
Renal ultrasound Renal ultrasound can help in the differential diagnosis of cases of red blood cells in the urine that are not due to glomerular causes or distinguish causes of renal failure due to urinary tract obstruction from renal failure due to disease. glomerular management.
In addition, considering the morphology and size of the kidney also helps to determine whether the disease progression is acute or chronic.

Kidney biopsy for histopathology has diagnostic value in determining the cause, type as well as the advanced stage of the disease. Besides the diagnostic value of histopathology, it also orients the treatment.
4. Evolution of glomerular disease
Glomerular disease can develop in one of the following ways:
The disease is completely regressive or there is very little protein/red blood cells in the urine: Most cases of post-streptococcal glomerulonephritis (especially children ) and about one-third of cases of IgA nephropathy. Chronic progressive disease causes fibrosis damage that gradually loses nephrons, creating chronic kidney disease with the final outcome being end-stage chronic renal failure requiring renal replacement therapy. The rate of progression depends on the cause of the disease and the course of treatment. In many cases, the disease progresses slowly about 20-25 years before reaching end-stage renal failure. Rapidly progressive disease: The disease is characterized by very rapid kidney failure, the kidneys can be completely destroyed within a few weeks to a few months if there is no treatment intervention. Histopathological picture is characterized by diffuse sickle-shaped lesions (due to cell proliferation and inflammatory cell infiltration) leading to glomerular necrosis and destruction. Therefore, the role of kidney biopsy in histopathological diagnosis is very important.
5. Treatment of glomerular disease
Treatment regimen depends on the etiology of glomerulonephritis
Specific treatment: For glomerular diseases where the disease-causing mechanism is the immune mechanism, corticosteroids or immunosuppressive drugs will be used. Rapidly progressive cases of glomerulonephritis sometimes require plasmapheresis to remove immune factors. Treatment of the underlying condition: Blood glucose control with diabetic glomerulopathy. Antibiotic treatment of post-infectious glomerulonephritis. Anticancer drug therapy or marrow transplantation with primary multiple myeloma or amyloid. Treatment of hypertension: Control of blood pressure (<130/80 mmHg) with antihypertensive agents is of particular importance for all types of glomerular disease. Good control of blood pressure will reduce damage to the glomeruli as well as slow the progression of chronic kidney disease. Vinmec International General Hospital is one of the hospitals that not only ensures professional quality with a team of leading doctors, modern equipment and technology, but also stands out for its examination and consulting services. and comprehensive, professional medical treatment; civilized, polite, safe and sterile medical examination and treatment space. Customers when choosing to perform tests here can be completely assured of the accuracy of test results.
If you notice any unusual health problems, you should visit and consult with a specialist.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.