This is an automatically translated article.
Posted by Master, Doctor Mai Vien Phuong - Department of Examination & Internal Medicine - Vinmec Central Park International General Hospital
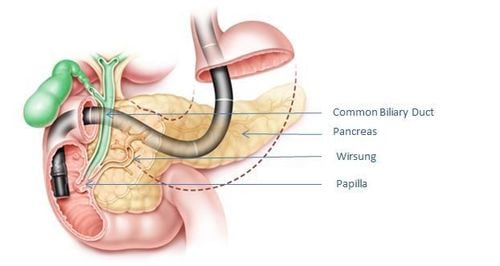
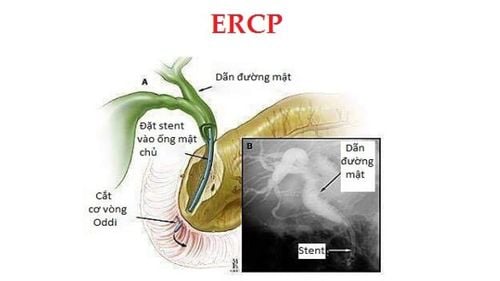
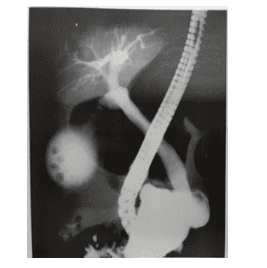
Endoscopic retrograde cholangiopancreatography (ERCP) is performed by a gastroenterologist or surgeon who has specialized training in this technique. The bronchoscope is a long, flexible tube with a light and camera on the end. Because the procedure involves sedation or general anesthesia, the patient will be consulted by an anesthesiologist before the procedure.
1.Prepare the patient
Preparing the patient for endoscopic retrograde cholangiopancreatography is straightforward. Patients need to fast and not put anything in their mouth including liquid for at least 6-8 hours before the procedure. It is customary to prepare a patient for endoscopic retrograde cholangiopancreatography. If performed in the morning, do not give the patient anything to eat from midnight. But if the procedure is performed in the afternoon, it may allow the patient to drink liquids early in the morning and then eat nothing after 8:30 a.m. Patients should also be allowed to take medications if they must take them within 2g of the procedure (with very little water, of course). This requires emphasis and attention because the procedure often involves the use of intravenous anesthetic.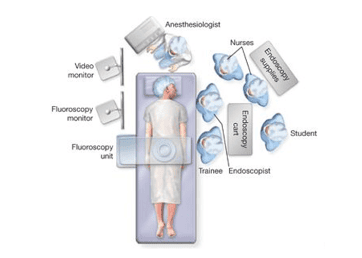

Pain relief, conscious pain control Although there are many good antispasmodic, analgesic and anesthetic drugs, doctors often use 2 things Buscopan 5mg and Valium 10mg TM. These drugs are dosed to the extent that analgesia is consciously sedated but with the complete cooperation of the patient. Recently, with critically ill patients, comatose patients require endotracheal anesthesia with the help of anesthesiologists as well as many newer pre-anesthetic drugs. Since then, all anesthetics and anesthetics used for patients with endoscopic retrograde cholangiopancreatography are completely decided by the anesthesiologist. Careful physical exploration can be combined with mechanical testing such as BP measurement, cardiac probe, pulse oximetry. This is very important and necessary for the safe endoscopic retrograde cholangiopancreatography. Anesthesiologists on duty when performing endoscopic retrograde cholangiopancreatography require close exploration, especially in at-risk patients. Pulse oximetry (Sp0)) is not currently mandatory, but it can be of great help in probing the patient's vital signs.
However, probes are not a complete substitute for visual monitoring and clinical examination. Intranasal oxygen has become more routine and helps maintain satisfactory oxygen saturation, especially in elderly patients to avoid unresponsiveness after the first dose of sedative analgesia. The antispasmodic Glucagon has long been the standard drug for anti-motility because the antispasmodic effect of glucagon is very good and it has been found that a dose of less than 1mg of Glucagon still has the same effect as a dose of 1g. . It is possible to repeat injection but the total dose should not exceed 0.5g if there is a case of long-term retrograde cholangiopancreatography. After inserting the bronchoscope through the duodenum, the assistant usually administers 0.25g of Glucagon to the infusion fluid. In addition, Atropin may be necessary in patients with duodenal spasm but poorly responding and is currently rarely used while other antispasmodics such as Buscopan, Cystabon ... although not as good as Glucagon, Cheap and widely used.
2.Patients will be monitored by monitoring during the procedure
All these drugs can affect blood pressure so it is best to monitor the patient's vital signs during the procedure. All patients, especially the elderly, because prolonged prone position can lead to hypoxemia, It is only recently that some potential dangers of intravenous analgesia have begun to be recognized. patients undergoing endoscopic cholangiopancreatoscopy, which occurs mostly in elderly patients.
Although these additional probes are not part of the standard requirements for endoscopic cholangiopancreatography, monitoring is recommended for general use because many therapeutic procedures are performed in elderly patients who are placed in the prone or nearly prone position for long periods of time. Therefore, careful exploration and strict adherence to the strict indications for endoscopic retrograde cholangiopancreatography should be followed by good patient preparation and a thorough examination of all endoscopic probes and instruments. The ablation machine before the start of the procedure not only provides good prevention of possible complications for the patient, but also helps the endoscopist to have success during the procedure.
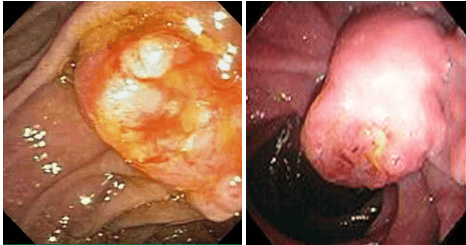
Performing ERCP procedure at Vinmec International General Hospital allows endoscopic diagnosis and treatment under sedation safely, helping patients no longer fear endoscopy with the most modern technical machines; The Department of Endoscopy is designed for patient privacy, comfort and safety. In addition, strict adherence to the principles of sterilization and disinfection is required to prevent the spread of pathogens through endoscopes to patients and medical staff. Fully equipped with facilities and equipment to allow endoscopic diagnosis and treatment under sedation, helping patients not feel pain and stimulation when performing the procedure; The ERCP procedure uses a modern flexible endoscope system, Endocut's electric knife has the advantage of not causing pancreatitis, pancreatic reaction; The implementation time is fast, safe, there are few complications with the success rate > 98%; A team of reputable doctors with extensive experience In addition to the strict adherence to the principles of sterilization and disinfection to prevent the spread of pathogens through endoscopes for patients and medical staff, exposure to harmful disinfectant chemicals, as well as ensure the patient's privacy, comfort and safety when going to the endoscopy. After the procedure, the patient is closely monitored by a team of professional medical staff, complications can be detected early for timely treatment.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.