This is an automatically translated article.
Posted by Master, Doctor Mai Vien Phuong - Department of Examination & Internal Medicine - Vinmec Central Park International General HospitalPeripapillary diverticulum is often closely related to the segment and the common bile duct and pancreatic duct, removing it can be a risky process. Fortunately, they often have a wide neck (mouth). These diverticula themselves are asymptomatic, but if they are located adjacent to the large duodenal papilla, they will affect the hepatopancreatic ball, especially when the diverticulum is located above the ceiling of the duodenal papilla, making catheter placement difficult. this is a contributing factor to catheter failure) or perforation during endoscopic sphincterotomy.
1. The diverticulum around the Vater papilla in the duodenum
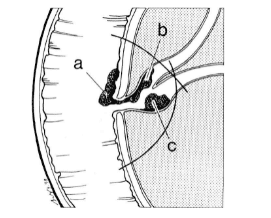
Peripapillary diverticulum may have one, two or three, posing the problem of identifying the papilla and correctly orienting this structure for endoscopic access.
According to the authors, endoscopic retrograde cholangiopancreatoscopy revealed the presence of a duodenal diverticulum in about 20%.” Assessing the papilloma in this setting can be difficult and requires guidelines for its access such as: The bronchoscope should be in a short route with the prone position more favorable to identify the papillae and give a biliarypancreatogram.If more than one diverticulum is present, the bronchoscope should be positioned short (60- 65 cm) allows identification of the diverticulum and the location of the papilla. The longitudinal fold will be visible toward the diverticulum, confirming that the papilla is located within the diverticulum. Furthermore, the papillae is almost never located within the diverticulum. , which is usually located above the Vater papilla, one can use this property to identify the large papillae because sometimes when the papilla is not found, one must now rule out whether it is located in D1, D. or in the pouch. If there is a diverticulum, it will be located between the end of the diverticulum to the papillae.
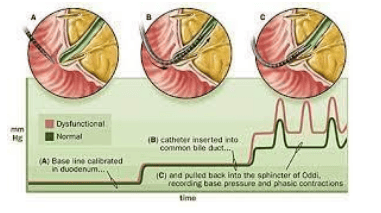
2. Sphincter dysfunction
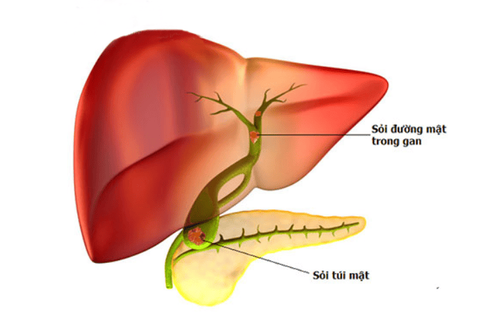
Sphincter dysfunction caused by abnormal anatomical changes or changes associated with a parapapillary diverticulum. The presence of a foreign body (bezoar) can disrupt the drainage of the bile-pancreatic duct and can cause biliary colic and acute pancreatitis. If the papilla is located below the diverticulum adjacent to the diverticulum wall, similar dysfunction will occur. This phenomenon can be identified by carefully examining the papilla and studying its activity during peristalsis. Peristalsis can compress the diverticulum and eventually cause physiological dysfunction of the papillary muscle. Therefore, sphincterotomy can be performed to prevent this from occurring, especially if biliary tract dilatation is present and liver dysfunction is present.
3. Polyps in Vater .'s shadow
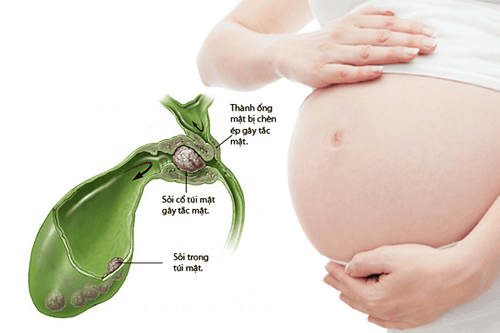
Peribulal lesions such as ductal adenomas or polypoid lesions can cause intermittent biliary tract disorders. A pedunculated polyp, the legs are quite wide enough to cause obstruction of the gastric outlet when the polyp prolapses into the stomach, and otherwise, the base of the polyp can cause temporary obstruction of the pancreatic duct and cause pancreatitis. .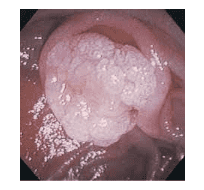
It is important for the endoscopist to determine that both bile and pancreatic ducts are not within the base of the polyp before considering polypectomy. This important structure is often located in the base of the polyp and serious complications will occur after polyp removal requiring surgical or endoscopic intervention. The author suggested that before resection of polyps in the peripapillary region, a diagnostic retrograde cholangiopancreatoscopy should be performed to identify the duct system. Once this important structure is identified, polypectomy can be performed.
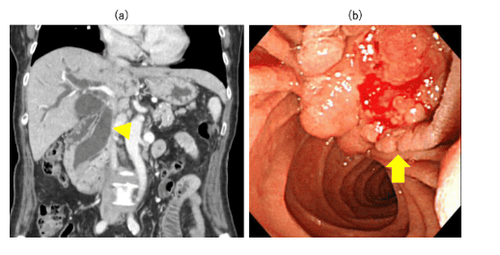
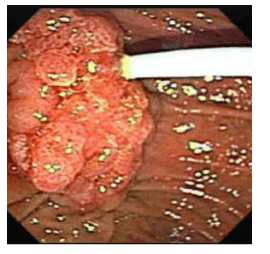
4. Cancer ball Vater
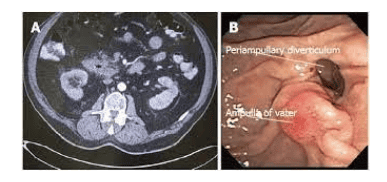
Vater papillary tumors usually cause very low biliary obstruction and sometimes a short papillary obstruction of the pancreatic duct. Patients with ampulla of Vater often present with obstructive jaundice and sometimes acute pancreatitis. If surgical indications are not considered in patients with Vater papillary cancer, treatment should be attempted to decompress one or two biliary-pancreatic systems. But usually only biliary decompression, because jaundice is the main complication of Vater papillary cancer. Here are a few different endoscopic images showing cancer (carcinoma) of the ampulla of Vater and only duodenoscopy can give the clearest picture.
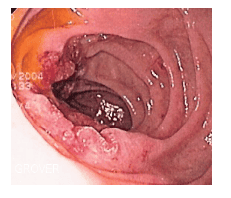
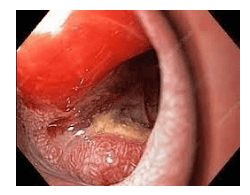
5. Duodenal cancer
There are ulcerative lesions but are indirect images of invasive carcinoma. Lesions are ulcerated plaques of the duodenum often associated with invasive pancreatic tumors. Its presence can add to the difficulty of endoscopic procedures, thus requiring mastery skill and patience for the correct diagnosis and decompression therapy. Thorough investigation of any duodenal lesion is of great management significance, multiple biopsies must be performed to confirm the diagnosis, and ultimately surgical or interventional radiology or endoscopic therapy may suggest stenting. treatment to relieve jaundice) for temporary prolongation. Obviously, the best method for identifying papillary lesions is endoscopy. Many authors advocate the use of retrograde cholangiopancreatography for this purpose, because the lesion is directly visualized on the surface of the tumor and can be biopsied.
6. What should be paid attention to in patients with biliary obstruction due to tumor obstructing the ampulla of Vater?
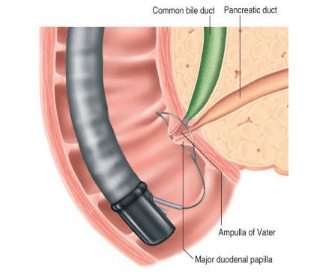
The endoscopist encountered a cancer causing biliary obstruction in a patient with ampullary cancer of Vater who had liver metastases. Endoscopy in treated jaundice should take into account coagulation function and may provide additional information about the pathological process, such as evidence of esophageal varices as a secondary manifestation of hypertension. Portal venous force or identification of ulcerative lesions has proven to be the cause of severe gastrointestinal bleeding, especially in patients with jaundice. This has made a very important contribution to the treatment and monitoring of patient care. However, the endoscopist should use a lateral viewoscope to examine the duodenum and the ampulla of Vater, because the straight view bronchoscope does not allow a complete examination of the D2 segment because the ampulla of Vater is only seen in a tangential fashion. and the surface is rarely directly visible, making the survey incomplete and the papillae not directly visible.
7. It is recommended to use a straight-line bronchoscope before using a lateral bronchoscope to evaluate the ampulla of Vater
If the endoscopist feels it is advantageous to use the bronchoscope to fully examine the esophagus and stomach, he or she may complete the bronchoscope examination and then perform the bronchoscope examination. side to survey needs and order information later. From experience, when using a straight-line scope, the incorrect orientation of the structures in the duodenum leads to an inappropriate diagnosis. For example, a lesion that appears to be the ball of Vater when viewed with a straight bronchoscope is actually a tumor-like lesion of the duodenal wall when examined with a lateral view.
Conclusion The endoscopist should establish a good relationship with a good radiographer as well as with a surgeon if the endoscopist is a gastroenterologist because these people are capable of assisting or directing. Continue to depressurize at the beginning or during the procedure. Cultivating such a supportive relationship is important in establishing a biliary-pancreatoscopy center. If the endoscopist is experienced in performing percutaneous biliary drainage but is unable to perform endoscopic decompression, the patient can be repositioned to the appropriate table position and allow catheterization to be performed. Percutaneous Transhepatic Biliary Drainage (PTBD) Thus, the endoscopist can devise a management strategy that avoids unnecessary surgical intervention, which can be caused by the endoscopist's inexperience in therapeutic endoscopy (endoscopic surgery) or endoscopy. failed search.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.