This is an automatically translated article.
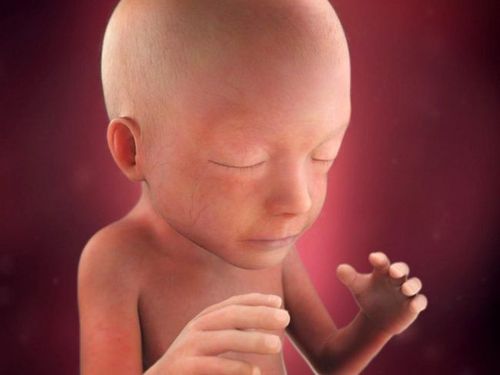
When a woman and her baby carry different Rhesus (Rh) protein factors, the condition is called Rh incompatibility or Rh factor incompatibility. This condition occurs when the mother is Rh negative and the fetus is Rh positive.1. How does the Rh factor affect pregnancy?
The Rh factor is a specific protein found on the surface of red blood cells. Like the ABO blood group, the Rh blood group is inherited from the parents' genes. Most people are Rh(+), but a small percentage are Rh(-) because they don't have the Rh protein.The positive or negative symbol after your blood type indicates your Rh factor. For example: Blood group listed as AB+ recorded in your medical record means that you have blood type AB and Rh(+) or Rh positive.
Rh factor does not directly affect your health, however, Rh factor plays a very important role during pregnancy. If a woman is Rh(-) and the fetus is Rh(+), the mother's body will treat the fetus' Rh(+) protein as foreign, so if the mother's immune system continues to When exposed to the baby's blood during pregnancy, labor and delivery, the mother's immune system produces antibodies against the baby's red blood cells. Antibodies are part of the body's immune system and they destroy foreign substances.
The antibodies produced are not a problem in the first pregnancy. The bigger concern is with subsequent pregnancies of the same woman. If the next fetus is Rh(+), these Rh antibodies can cross the placenta and destroy the baby's red blood cells. This can lead to life-threatening anemia in the fetus, a condition in which red blood cells are destroyed faster than the baby's body can produce red, while red blood cells Demand plays an extremely important role to carry oxygen throughout the body and nourish the fetus.
Therefore, Rh(-) pregnant women are advised to have some other blood tests such as antibody screening tests during the first trimester of pregnancy, during the 28th week of pregnancy and at delivery. Antibody screening tests are used to detect antibodies against Rh(+) blood. If you have not started producing Rh antibodies, you may need an injection of a blood product called Rh immune globulin. Immunoglobulins prevent the mother's body from producing Rh antibodies during pregnancy. If the baby is born with Rh(-) blood type, no additional treatment is needed, and if the baby is born Rh(+), you will need another shot soon after birth.
If the woman is Rh(-) and the fetus may be Rh(+), the doctor may recommend Rh immune globulin injections in situations where the mother's blood may come into contact with fetal blood, including:
Miscarriage Abortion Ectopic pregnancy - when a fertilized egg implants and implants outside the uterus, usually in a fallopian tube Molar pregnancy, which is a non-cancerous (benign) tumor development in the uterus Amniocentesis - a prenatal test in which a sample of the fluid that surrounds and protects the baby in the uterus (amniotic fluid) is removed for testing or treatment Sampling for a chorionic villus sampling Test prenatal genetic testing (English name is Cordocentesis), also known as percutaneous umbilical cord blood sampling (PUBS). Blood is taken from a vein in the umbilical cord to check for chromosomal abnormalities. Doctors usually perform this test when the fetus is 18 weeks old. This test carries a higher risk of miscarriage than amniocentesis or chorionic villus sampling. In general, this test is done only when the results of other tests are not clear. Bleeding during pregnancy Abdominal trauma during pregnancy The doctor or midwife performs manual fetal rotation before labor During childbirth bleeding and contact between mother and baby's blood If the antibody screening test shows that the mother has produced antibodies, the injection of Rh immune globulin will not be effective. The fetus and the mother will be carefully and closely monitored. The person can receive a blood transfusion through the umbilical cord during pregnancy, if necessary, the fetus can receive a blood transfusion through the umbilical cord or shortly after birth.

Thử nghiệm di truyền trước sinh
2. What are the symptoms of Rh incompatibility?
Symptoms of Rh incompatibility in the fetus can range from mild to life-threatening. When maternal antibodies attack the baby's red blood cells with symptoms of hemolytic disease, this means that the baby's red blood cells are being destroyed and leads to a buildup of bilirubin in the blood.Bilirubin is a chemical produced from the breakdown of red blood cells. Too much bilirubin is a sign that the liver is having trouble processing old blood cells.
The baby may have one or more of the following symptoms if the bilirubin level is high after birth:
Jaundice and scleral jaundice Lethargy Low muscle tone These symptoms should subside after Rh incompatibility treatment success.
3. Who is at risk for Rh incompatibility?
Any woman who is Rh negative and whose husband is Rh positive or has an unspecified Rh status is at risk for an Rh incompatible pregnancy. However, due to the low percentage of people with Rh(-) blood type in the community, this disease does not occur often.The body takes time to develop antibodies, so the first child is usually affected. However, if a mother becomes susceptible because of a miscarriage or abortion, her own first live birth may be affected because she has already produced antibodies and develops Rh incompatibility. .
Once the mother may be exposed to Rh positive blood during prenatal tests or procedures, eg amniocentesis. In this test, the doctor uses a needle to remove some fluid from the amniotic sac to check for problems in the developing fetus.
4. How is Rh incompatibility diagnosed?

Xét nghiệm máu để xác định tình trạng Rh của sản phụ
If the woman is Rh(-) during pregnancy, the husband can also be tested to determine the blood type. If the woman's husband is also Rh(-), there is nothing to worry about. If the husband is Rh(+), the doctor will look for signs of Rh incompatibility such as:
The indirect Coomb test is used to find out if a serum sample has antibodies against a particular type of red blood cell and This technique also identifies potential unagglutinated antibodies in the sample of interest (Figure 11). This test is performed by incubating red blood cells with a serum sample, washing to remove any unbound antibodies and then adding a second anti-antibody to conjugate the cells. A higher than normal bilirubin level in a newborn's blood is a sign of Rh incompatibility. In a full-term baby less than 24 hours, bilirubin levels should be less than 6.0 milligrams per deciliter (dL). Signs of red blood cell destruction in the infant's blood may indicate Rh incompatibility. This can be determined by the shape and structure of the red blood cells when examined under a microscope. In addition, the doctor may test the baby's blood for maternal antibodies that are breaking down the baby's red blood cells.
5. How is Rh incompatibility treated?
Treatment focuses on blocking the effects of Rh incompatibility. In mild cases, the baby can be treated after birth as follows:Blood transfusions Hydrating fluids Electrolytes Phototherapy Phototherapy is the most common treatment for lowering bilirubin levels (the cause neonatal jaundice). Jaundice lamp is a low cost, high performance and compact device that can provide high intensity light to help improve hyperbilirubinemia. Depending on the child's condition, this technique may be repeated until the Rh antibodies are gone and the excess bilirubin has been removed from the child's blood.
If you are pregnant and your doctor determines that you have developed antibodies against your baby, your pregnancy will be closely monitored.
You can prevent the effects of Rh incompatibility by injecting Rh immune globulin (RhIg) during the first trimester, during a miscarriage, or during bleeding during pregnancy. This blood product contains antibodies to the Rh factor. If the fetus is Rh positive, the mother should get a second dose a few days after delivery.
In very rare and severe cases, umbilical cord blood transfusion can be performed while the fetus is still in the uterus or after birth. However, due to the success of RhIg injections, this treatment is performed in less than 1% of Rh-incompatible women in the United States.
6. Complications of Rh . Incompatibility

Có những biến chứng nào của không tương thích Rh?
Damage to the baby's brain, called kernicterus, Child with fluid buildup Children with problems with mental health, mobility, hearing and speech Convulsions Anemia Heart failure Death
If you have unusual symptoms, you should be examined and consulted with a specialist.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
Article referenced source: Healthline.com