This is an automatically translated article.
Rh incompatibility occurs when a pregnant mother with Rh negative blood group is exposed to Rh positive blood from the fetus, leading to the development of Rh antibodies in the mother's body. This causes the fetus to become anemic, which can lead to hemolytic disease of the newborn. In severe cases can lead to death. Therefore, every pregnant woman needs an Rh test during pregnancy.1. What is blood group?
Each drop of blood contains red blood cells, which carry oxygen throughout your body; In addition, blood also contains white blood cells that help the body fight infections and platelets that play an important role in blood clotting.But that's not all components of the blood. Your blood also contains antigens, which are proteins and sugars located on the surface of red blood cells, and this is how scientists classify each person's blood type. While there are at least 33 blood grouping systems, in clinical practice only two are widely used. These are the ABO and Rh positive/Rh negative blood group systems. Together these two systems form the eight basic blood types that most people are familiar with:
Blood group A positive Blood group A negative Blood group B positive Blood group B negative Blood group AB positive Blood group AB negative Blood group O positive Blood group O negative Blood group The same for the case of pregnant mother with Rh negative blood group like mother O Rh- blood group during pregnancy, O Rh+ blood group during pregnancy, blood group B Rh+ during pregnancy ....

2. Why is Rh pregnancy test needed?
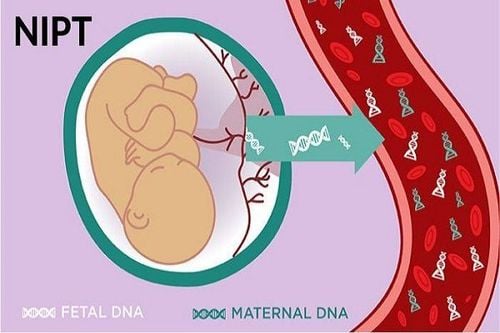
During pregnancy, problems can occur if the mother is Rh(+) and the fetus is Rh(-) which is called mother-child blood type incompatibility. Normally, the mother's blood does not mix with the fetal blood during pregnancy. However, a small amount of your baby's blood can come into contact with your blood during delivery or if you have bleeding or abdominal trauma during pregnancy. If you are Rh(-) and your baby is Rh(-), your body may make proteins called Rh antibodies after coming into contact with your baby's red blood cells.
The antibodies produced are not a problem in the first pregnancy. The bigger concern is with subsequent pregnancies of the same woman. If the next fetus is Rh(+), these Rh antibodies can cross the placenta and destroy the baby's red blood cells. This can lead to life-threatening anemia in the fetus, a condition in which red blood cells are destroyed faster than the baby's body can produce red, while red blood cells Demand plays an extremely important role to carry oxygen throughout the body and nourish the fetus.
Therefore, Rh(-) pregnant women are advised to have some other blood tests such as antibody screening tests during the first trimester of pregnancy, during the 28th week of pregnancy and at delivery. Antibody screening tests are used to detect antibodies against Rh(+) blood. If you have not started producing Rh antibodies, you may need an injection of a blood product called Rh immune globulin. Immunoglobulins prevent the mother's body from producing Rh antibodies during pregnancy. If the baby is born with Rh(-) blood type, no additional treatment is needed, and if the baby is born Rh(+), you will need another shot soon after birth.
If the woman is Rh(-) and the fetus may be Rh(+), the doctor may recommend Rh immune globulin injections in situations where the mother's blood may come into contact with fetal blood, including:
Miscarriage Abortion Ectopic pregnancy - when a fertilized egg implants outside the uterus, usually in a fallopian tube Molar pregnancy, which is a non-cancerous (benign) tumor development in the uterus Amniocentesis - a prenatal test in which a sample of the fluid that surrounds and protects the baby in the uterus (amniotic fluid) is removed for testing or treatment Sampling for a chorionic villus sampling Test prenatal genetic testing (English name is Cordocentesis), also known as percutaneous umbilical cord blood sampling (PUBS). Blood is taken from a vein in the umbilical cord to check for chromosomal abnormalities. Doctors usually perform this test when the fetus is 18 weeks old. This test carries a higher risk of miscarriage than amniocentesis or chorionic villus sampling. In general, this test is only done when the results of other tests are not clear Bleeding during pregnancy Abdominal trauma during pregnancy The doctor or midwife performs manual fetal rotation before labor During childbirth bleeding and contact between mother and baby's blood If the antibody screening test shows that the mother has produced antibodies, Rh immune globulin injections will not be effective. The fetus and the mother will be carefully and closely monitored. The person can receive a blood transfusion through the umbilical cord during pregnancy, if necessary, the fetus can receive a blood transfusion through the umbilical cord or shortly after birth.
Trắc nghiệm: Bạn có hiểu đúng về dấu hiệu mang thai sớm?
Các dấu hiệu mang thai sớm không phải chỉ mỗi trễ kinh mà còn có rất nhiều dấu hiệu khác như xuất huyết âm đạo, ngực căng tức,… Điểm xem bạn biết được bao nhiêu dấu hiệu mang thai sớm thông qua bài trắc nghiệm này nhé!
3. How to prevent mother-child blood group incompatibility?
3.1 Anti-D Immunoglobulin Vaccination Anti-D Immunoglobulin neutralizes any RhD-positive antigens that may have entered the mother's bloodstream during pregnancy. If the antigens have been neutralized, the mother's blood will not produce antibodies against the fetal red blood cells.The mother will be vaccinated with anti-D Immunoglobulin if the doctor suspects that the woman is at risk of RhD antigens from the fetus having entered the mother's blood in the case of bleeding and invasive procedures. such as amniocentesis) or if abdominal trauma.
Anti-D Immunoglobulin vaccination is also indicated in the third trimester of pregnancy if the mother's blood group is RhD negative. This is because there is a chance that a small amount of blood from the fetus will enter the mother's bloodstream during this time.

3.2 Routine anti-D prophylaxis before delivery There are currently two ways for pregnant women to receive anti-D Immunoglobulin
1 dose regimen: Immunoglobulin is given to women during the 28th to 30th week of pregnancy. 2 dose treatment: The mother will receive 2 injections; one at 28 weeks and the other at 34 weeks of pregnancy Currently, there does not appear to be any difference in efficacy between 1-dose or 2-dose regimens.
3.3 When should pregnant women be vaccinated with anti-D Immunoglobulin? Vaccination against anti-D Immunoglobulin is recommended for all pregnant women with Rh(-) blood type who are not already sensitive to the RhD antigen, even if the woman has been previously vaccinated with anti-D Immunoglobulin. Because once vaccinated with anti-D Immunoglobulin will not protect the mother for life against rhesus disease, the mother needs a booster shot if she meets the necessary conditions to need a booster shot.
3.4 Anti-D Immunoglobulin vaccination after birth After birth, a blood sample of the newborn is taken from the umbilical cord. If the mother is RhD negative and the infant is RhD positive and she has not yet produced antibodies against Rh(+), she will be vaccinated with anti-D Immunoglobulin within 72 hours of delivery. will destroy any RhD(+) blood cells that have entered the mother's bloodstream during delivery. This means that the mother's blood will not have a chance to make antibodies and will greatly reduce the risk of a subsequent pregnancy with rhesus (also known as hemolytic disease of the newborn due to incompatibility). mother's blood).
3.5 Complications from Anti-D Immunoglobulin Some of the side effects that can be caused by an allergic reaction to an anti-D Immunoglobulin shot include a rash or flu-like symptoms. Although anti-D Immunoglobulin is produced from donor plasma and will be carefully tested and screened, but there may still be some but very small risks. However, the evidence of anti-D Immunoglobulin vaccination suggests that the benefits of preventing rhesus disease far outweigh these risks.
Therefore, when abnormal symptoms appear during pregnancy, you should be examined and consulted with a specialist.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
Article referenced source: nhs.uk