This is an automatically translated article.
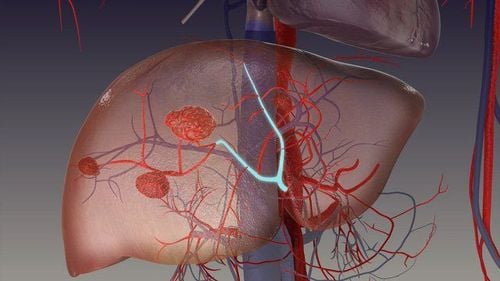
Posted by Doctor Mai Vien Phuong - Department of Medical Examination & Internal Medicine, Vinmec Central Park International General HospitalLiver hemangioma presents as an incidental finding during abdominal ultrasound and is described as a solitary or multiple lesion. Liver hemangiomas are classified according to their nature as cavernous, capillary and sclerosing hemangiomas; The latter are characterized by degeneration and replacement of fibers and may be misdiagnosed as melanoma.
1. Potential progression of liver hemangiomas
The natural progression of liver hemangiomas varies, previously these lesions were considered stable. However, many studies have shown progression and increase in size when followed over the course of many years. In a study of 236 patients with a median follow-up of 48 months (3-26), 61% experienced an increase in hemangioma size with the highest rate of increase when hemangioma was 8- 10 cm (0.80 ± 0.62 cm/year) and in younger patients over 30 years of age.
In another study with 123 patients (163 hepatic hemangiomas), the rate of increase was 50.9% by any number in the mean absolute linear size at an annual growth rate of 0.03 cm for all lesions and 0.19 cm for those growing >5%. This study also found a correlation with an increase in annual growth in liver hemangiomas 5 cm or more at baseline. They predicted an annual growth rate for all liver hemangiomas of 0.34 mm
2. Diagnosis of liver hemangioma
Unique features of hepatic hemangioma by imaging are the presence of peripheral nodular enhancement and progressive afferent filling. Ultrasound (USA), computed tomography (CT), and magnetic resonance imaging (MRI) are the most common imaging tests. Atypical lesions may require more than one imaging test.
Abdominal ultrasound is often the first diagnostic imaging test due to its availability. Hepatomegaly appeared as a well-defined, homogeneous hyperechoic mass with posterior acoustic enhancement (Figure 1). Color-Doppler US does not improve diagnostic accuracy because it only displays blood flow in hepatic hemangiomas with intraportal shunts.
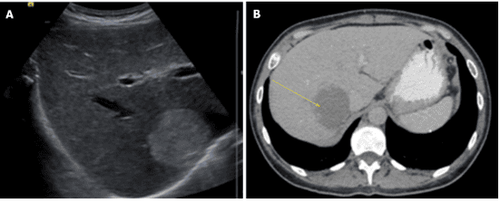
Abdominal ultrasound has a sensitivity of 96.9% and a specificity of 60.3%. Some malignant liver lesions (hepatocellular carcinoma and liver metastases) may produce similar sound patterns and a different imaging modality must be used to confirm the diagnosis.
Contrast-enhanced United States (CEUS) uses microscopic bubbles filled with gas to describe the signal produced by blood flow. Hepatic hemangioma shows peripheral nodular contrast enhancement in the early (arterial) stage with afferent filling in the later stages.
Several studies have demonstrated that CEUS improves the characteristics and specificity for the diagnosis of HH.
CT has a sensitivity of 98.3% and a specificity of 55%. Liver hemangiomas are described as well-defined hypodense masses. When contrast is used, peripheral nodular enhancement with radial uniform filling is expected, however small lesions and liver hemangiomas with areas of cysts, fibrosis, or thrombosis may show an atypical form.
MRI shows a well-defined, smooth, homogeneous lesion, reduced T1 score and increased T2W score Some malignancies may show similar intensities on T2, to distinguish liver hemangiomas from In solid cancerous liver lesions, the echo time increases, causing the signal from the malignant lesion to decrease and the signal from the liver hemangioma to increase. Administration of gadolinium showed peripheral enhancement of the arterial phase and kept the contrast in the slow phase, allowing it to be distinguished from hypertensive tumors that often have slow-washing contrast. MRI has been considered the best imaging modality for liver hemangiomas with a sensitivity of 90%-100% and a specificity of 91%-99%.
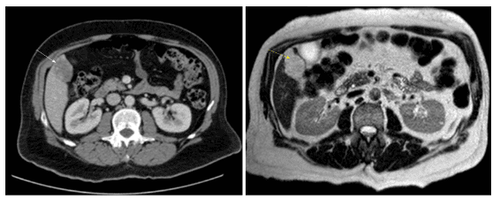
Angiography is the best option for atypical liver hemangiomas that are difficult to diagnose with other imaging tests. Liver hemangiomas present as “snow trees” or “cotton balls” with large vessels and diffuse contrast accumulation that continues into the late phase. Technetium-99m pertechnetate-labelled red blood cell pool scintigraphy, single photon emission computed tomography, and positron emission tomography/CT are other imaging modalities available for the diagnosis of hepatic hemangiomas in these patients. have atypical tumours, history of chronic liver disease or malignancy.
Needle aspiration biopsy is not recommended because of the high bleeding risk and low diagnostic yield.
3. Conclusion
Most liver hemangiomas are diagnosed incidentally on imaging tests because most patients are asymptomatic throughout their lives. Patients with symptoms are usually due to larger lesions.
Over the years, nonsurgical minimally invasive procedures for tumor reduction and laparoscopic surgery have shown good results in selected patients.
Rarely for liver hemangiomas present with life-threatening conditions such as acute traumatic rupture or coagulopathy. Only in these cases can urgent surgical management be warranted.
Currently, Vinmec International General Hospital has Hepatobiliary Screening packages, which help detect Hepatitis Virus at an early stage even when there are no symptoms. In addition, the comprehensive hepatobiliary screening package helps customers:
Evaluate the liver's ability to work through liver enzyme tests; Evaluation of bile function; vascular nutrition; Early screening for liver cancer; Perform tests such as Total blood cell analysis, blood clotting ability, screening for hepatitis B, C Assessment of liver and biliary status through ultrasound images and diseases that are at risk of affecting liver disease / liver disease. more severe liver disease In-depth analysis of parameters to evaluate hepatobiliary function through laboratory and subclinical; the risk of affecting the liver and early screening for hepatobiliary cancer.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
References
Ishak KG, Rabin L. Benign tumors of the liver. Med Clin North Am . 1975;59:995-1013. [PubMed] [DOI] Yang Z, Tan H, Liu X, Sun Y. Extremely Giant Liver Hemangioma (50 cm) with Kasabach-Merritt Syndrome. J Gastrointest Surg . 2017;21:1748-1749. [PubMed] [DOI] Schumacker HB. Hemangioma of the liver: discussion of symptomatology and report of patient treated by operation. Surgery . 1942;11:209–222. Reddy KR, Kligerman S, Levi J, Livingstone A, Molina E, Franceschi D, Badalamenti S, Jeffers L, Tzakis A, Schiff ER. Benign and solid tumors of the liver: relationship to sex, age, size of tumors, and outcome. Am Surg . 2001;67:173-178. [PubMed] Hasan HY, Hinshaw JL, Borman EJ, Gegios A, Leverson G, Winslow ER. Assessing normal growth of hepatic hemangiomas during long-term follow-up. JAMA Surg . 2014;149:1266-1271. [PubMed] [DOI] Monica Leon, Luis Chavez, Salim Surani, Hepatic hemangioma: What internists need to know, World J Gastroenterol. Jan 7, 2020; 26(1): 11-20