This is an automatically translated article.
Posted by Doctor Mai Vien Phuong - Department of Examination & Internal Medicine, Vinmec Central Park International General Hospital
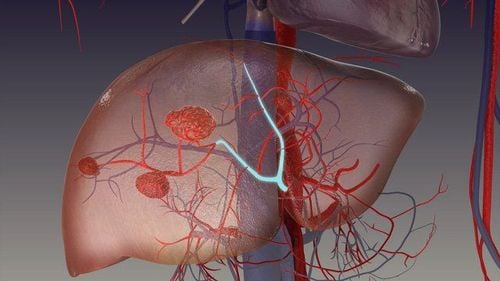
Hepatic hemangioma (HH) is a tumor of dermis origin consisting of a blood-filled space, nourished by the hepatic arterial circulation and lined by a flat layer of endothelial cells. This is the most common benign liver tumor, presenting as a well-described proliferative lesion, commonly seen in women with an incidence ranging from 0.4% to 7.3% (based on on autopsy results) and the prevalence is 0.4%-20% in the general population.
1. Overview
Hepatic hemangioma (HH) is the most common benign liver tumor and it is often discovered incidentally during physical examinations. This tumor arose from a vascular malformation; however, the pathophysiology has not yet been elucidated. Symptoms often correlate with the size and location of the tumor. Less commonly, the presence of a large hemangioma can cause life-threatening conditions.
Diagnosis can be established by identifying signs of liver hemangioma in several imaging tests. In patients with abdominal symptoms, other causes should be ruled out first before attributing hepatic hemangioma as the cause. For asymptomatic patients, no treatment is needed and follow-up is usually reserved for hemangiomas larger than 5 cm.
2. Symptoms of liver hemangioma
Liver hemangiomas are usually asymptomatic, however symptoms may appear when the HH is larger than > 5 cm. Symptoms are nonspecific, and patients often describe right upper quadrant abdominal pain, discomfort, and fullness, secondary to distension and Glisson's cyst. There is a tumor > 10 cm with abdominal distention. The location of the liver mass can put pressure on and compress adjacent structures causing other symptoms such as nausea, early satiety, and postprandial bloating. Less common symptoms include fever, jaundice, dyspnea, high-output heart failure, and serum sickness.
Giant hemangioma can cause a life-threatening coagulation disorder known as Kasabach-Merrit syndrome (thrombocytopenia, disseminated intravascular coagulation, and systemic bleeding) with coagulopathy secondary to thrombocytopenia, anemia, decreased fibrinogenimia, decreased prothrombin time, and increased D-dimer. This syndrome has been reported with an incidence ranging from 0.3% of total HHs to 26% in tumors >15 cm.
Another serious complication is bleeding due to spontaneous rupture or trauma (in giant peripheral and peripheral lesions), however the risk is extremely low (0.47%)
3. Treatment of liver hemangioma
Small, asymptomatic liver hemangiomas do not require treatment or monitoring. Some authors suggest monitoring liver hemangiomas > 5 cm at 6-12 months to assess rapid growth with the same imaging tests used at diagnosis.
Treatment should be limited to patients who are symptomatic, with persistently growing masses, compression of adjacent organs (gastric outlet obstruction, Budd-Chiari syndrome) or complications such as rupture due to intraperitoneal bleeding or Kasabach-Merrit syndrome.
Abdominal pain should be carefully evaluated in patients with hemangiomas and other possible causes should be kept in mind before definitive treatment is decided. Farges et al diagnosed 87 patients with abdominal pain and hemangiomas, of which 54% were found to have other comorbidities due to abdominal pain. Specific treatment for abdominal pain and liver hemangioma was required in 14 patients, and half of them remained symptomatic after treatment, suggesting another cause of pain. In another study, the majority of patients with abdominal pain and liver hemangioma were found to have symptoms related to various gastrointestinal diseases (irritable bowel syndrome, gastroesophageal reflux disease, hepatitis). , peptic ulcer, gallbladder disease) and only 21.7% of patients have symptoms, abdominal pain is due to liver hemangioma.
3.1 Surgery Surgery continues to be the most common treatment for liver hemangiomas. Surgical management includes hepatectomy, nuclear transplantation, hepatic artery ligation, and liver transplantation. The most common procedures worldwide are liver resection and transplantation (open, laparoscopic or robotic).
The first hepatectomy for liver hemangiomas was performed in 1987 by Schwartz et al. and in 1988, Alper et al reported the first nine patients treated with granulation.
The choice of procedure depends on the size, number of lesions, location, surgeon's experience and facility resources. Both techniques yield minimal postoperative morbidity.
In recent years, a number of studies have evaluated nuclear separation compared with hepatectomy and most have concluded that puncture is associated with lower morbidity, shorter operative time, Less blood loss and fewer complications. However, when the liver hemangioma was larger than 10 cm, Zhang et al found no difference in operative time, blood loss, complications or hospital stay between surgery and resection.
Liver hemangioma surgery is technically easier in peripheral hemangiomas, when performed in central liver hemangiomas, the procedure causes longer vascular occlusion time, longer surgery time. and lose more blood. Central liver hemangiomas (Stages I, IV, V and VIII) were treated with an enlarged left and right hepatectomy. This therapy can remove 60% to 80% of liver parenchyma, leading to a higher risk of postoperative liver failure. Some lesions are suitable for meniscalectomy.
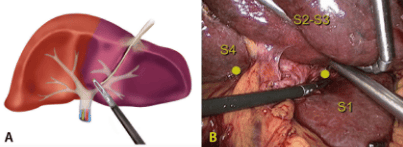
Improvements in laparoscopic surgery have increased the number of cases treated with minimally invasive surgery for nuclear resection or transplantation. Laparoscopic liver surgery is preferred in left-sided, small, and right-resectable lesions.
A recent retrospective study compared open and laparoscopic liver surgery for hemangiomas; The results support endoscopic therapy with less blood loss, lower complication rates, and shorter postoperative hospital stays. However, the baseline patient characteristics between the two groups were not equal as the surgeon decided to open or laparoscopic surgery based on tumor characteristics.
Liver transplantation for benign solid tumors is not considered a first-line treatment due to disease and lack of organs. A study published in 2015 analyzed data from the United Network of Organ Sharing from 1988 to 2013 and found 147 (0.17%) liver transplants in US patients performed for tumors. Benign tumors of the liver, including 25 transplants for liver hemangiomas.
Unresectable giant-specific liver transplantation for liver hemangiomas causing severe symptoms (respiratory failure, abdominal pain), failure of previous interventions, or life-threatening complications such as Kasabach-Merrit syndrome.
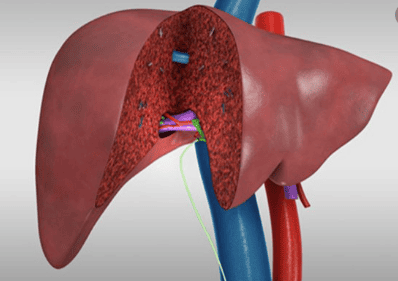
3.2 Treatment for Hemangiomas Non-surgical Peripheral artery embolization (TAE) is used to control acute bleeding or shrink liver hemangiomas before surgery with metal coils, gel beads, alcohol. polyvinyl and liquids such as N-butyl-2-cyanoacrylate, bleomycin-lipiodol. However, TAE is also used as a single treatment with acceptable results.
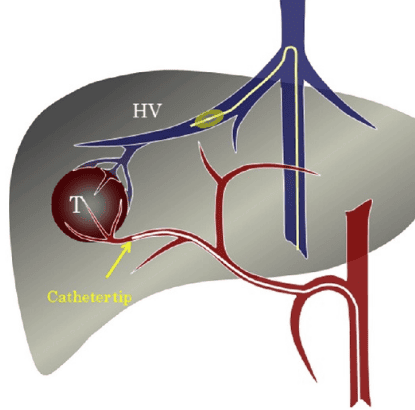
The pingyangmycin/lipiodol mixture was first studied as a single treatment for liver hemangiomas. Two studies reported good results with significant volume reduction for hepatic hemangiomas and reduction of symptoms. Pingyagmycin is available only in China, similar studies have been performed elsewhere with bleomycin as an alternative to pingyagmycin.
A study of 23 patients (29 for hepatic hemangioma) who were managed TAE with bleomycin-lipiodol concluded that 73.9% of patients had >50% volume regressing HH. Administration of Bleomycin leads to microthrombotic formation, leading to tumor atrophy and fibrosis. It also induces a nonspecific inflammatory process around the hepatic hemangioma and in the portal area. Acute liver failure, hepatic infarction, abscess, intrahepatic biloma, cholecystitis, splenic infarction, hepatic artery perforation, and sclerosing cholangitis have been reported as complications associated with TAE with Bleomycin.
Radiofrequency ablation (RFA) can be used percutaneously, endoscopically, or with open surgery. RFA induces thermal damage to vascular endothelial structures and promotes thrombus formation. RFA is usually performed according to US guidelines; Percutaneous RFA-guided CT is suitable for liver hemangiomas located deep in the liver parenchyma.
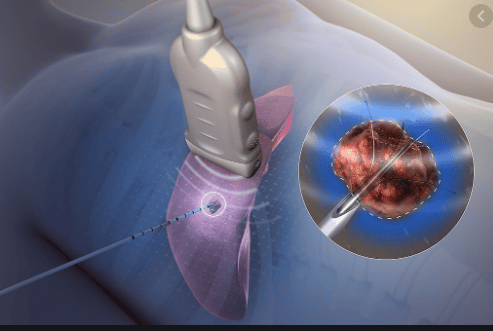
Endoscopic RFA with US guidelines is preferred for subcapsular hemangiomas. Laparoscopic RFA compared with open surgery is associated with shorter operative time, less pain, shorter hospital stay, and lower cost of hospital stay.
Prolonged RFA easily causes hemolysis, hemoglobinuria and acute kidney injury, so it is not suitable for large liver hemangiomas. Other complications of RFA include bleeding at the electrode entry site, rupture for hepatic hemangioma, and damage to nearby organs from puncture or thermal trauma.
The established indications for RFA in this population are maximal diameter of liver hemangioma > 5 cm, tumor enlargement > 1 cm within 2 years, persistent abdominal pain associated with hemangioma liver and exclude other GI diseases. Contraindications include patients with a tendency to heavy bleeding, malignancies, Kasabach-Merrit syndrome, infections (inflammation of the biliary system), low immune function, and severe organ failure.
The use of anti-VEGFs such as sorafenib and bevacizumab has been reported in case of incidental reports of reduced size for liver hemangiomas. A retrospective study aimed at investigating hemangiomas with anti-VEGF (bevacizumab or sunitinib) showed no significant volume reduction. Metformin has also been reported in a case report to reduce the size of a liver hemangioma randomly.
3.3 Liver transplantation with resection liver transplantation for liver hemangiomas In recent years, the criteria for donor liver transplantation have been expanded to overcome organ shortages. Partially resected liver donors for hemangiomas have been shown to be a viable source for liver transplantation with acceptable receptor outcomes and for non-progressive hemangiomas.
4. Conclusion
Most liver hemangiomas are diagnosed incidentally on imaging tests because most patients are asymptomatic throughout their lives. Patients with symptoms are usually due to larger lesions.
Since the natural history of liver hemangioma is benign and the progressive increase in size occurs in less than 40%, most patients can rest assured and just observe. When a patient has symptoms, the first step is to rule out other causes of their symptoms. Once other etiologies are excluded and liver hemangiomas are considered to be the cause of the symptoms, treatment modalities are determined based on the patient's size, anatomy, and comorbidities.
Over the years, non-surgical minimally invasive procedures for tumor reduction and laparoscopic surgery have shown good results in selected patients.
Rarely for liver hemangiomas present with life-threatening conditions such as acute traumatic rupture or coagulopathy. Only in these cases can urgent surgical management be warranted.
Clinicians should distinguish between observation and optimal management based on clinical presentation. If treatment is required, a minimally invasive approach should be pursued. Future research will help clinicians understand the pathogenesis of liver hemangiomas and guide management.
Currently, Vinmec International General Hospital has Hepatobiliary Screening packages, which help detect Hepatitis Virus at an early stage even when there are no symptoms. In addition, the comprehensive hepatobiliary screening package helps customers:
Evaluate the liver's ability to work through liver enzyme tests; Evaluation of bile function; vascular nutrition; Early screening for liver cancer; Perform tests such as Total blood cell analysis, blood clotting ability, screening for hepatitis B, C Assessment of liver and biliary status through ultrasound images and diseases that are at risk of affecting liver disease / liver disease. more severe liver disease In-depth analysis of parameters to evaluate hepatobiliary function through laboratory and subclinical tests; the risk of affecting the liver and early screening for hepatobiliary cancer
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
References
Ishak KG, Rabin L. Benign tumors of the liver. Med Clin North Am . 1975;59:995-1013. [PubMed] [DOI] Yang Z, Tan H, Liu X, Sun Y. Extremely Giant Liver Hemangioma (50 cm) with Kasabach-Merritt Syndrome. J Gastrointest Surg . 2017;21:1748-1749. [PubMed] [DOI] Schumacker HB. Hemangioma of the liver: discussion of symptomatology and report of patient treated by operation. Surgery . 1942;11:209–222. Reddy KR, Kligerman S, Levi J, Livingstone A, Molina E, Franceschi D, Badalamenti S, Jeffers L, Tzakis A, Schiff ER. Benign and solid tumors of the liver: relationship to sex, age, size of tumors, and outcome. Am Surg . 2001;67:173-178. [PubMed] Hasan HY, Hinshaw JL, Borman EJ, Gegios A, Leverson G, Winslow ER. Assessing normal growth of hepatic hemangiomas during long-term follow-up. JAMA Surg . 2014;149:1266-1271. [PubMed] [DOI] Monica Leon, Luis Chavez, Salim Surani, Hepatic hemangioma: What internists need to know, World J Gastroenterol. Jan 7, 2020; 26(1): 11-20