This is an automatically translated article.
The article was written by Doctor Mai Vien Phuong - Department of Medical Examination & Internal Medicine - Vinmec Central Park International General HospitalIn the United States, cirrhosis is the leading non-malignant cause of death in hepatobiliary-digestive diseases, with an annual mortality rate of about 30,000. Patients with cirrhosis often die from complications of portal hypertension. One of the most serious, common and fatal complications is rupture of esophageal varices as a result of portal hypertension.
Along with the development of gastrointestinal endoscopy, a number of recent studies have shown that cirrhosis is associated with the formation and progression of portal hypertension. In addition to the main picture of portal hypertension commonly seen on endoscopic examination of mucosal mosaicism, erosive lesions have also been detected in the stomach of cirrhotic patients and have been classified by some authors as a form of portal hypertension. In order to reduce the mortality rate in patients with cirrhosis, the prevention of bleeding due to ruptured esophageal varices plays a very important role. The first method is a non-selective beta blocker led by propranolol. Several studies have shown that propranolol reduces the rate of primary as well as secondary bleeding. However, the downside of propranolol is the potential for some side effects that limit its clinical use.
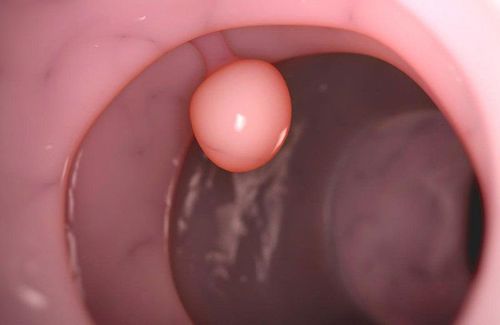
On the other hand, one of the more widely used treatment methods recently is endoscopic rubber band ligation of the esophageal varices due to its high safety and effectiveness.
1. Differential diagnosis of portal hypertension
BDDTAC needs to be differentiated from a type of lesion that can be seen in the setting of cirrhosis as “gastric vasodilatation” (GAVE). GAVE is defined endoscopically with a typical image of a collection of red dots in a band-shaped or diffuse pattern in the antrum, confirmed by histopathological findings with vasodilatation. Unlike BDDTAC, GAVE did not improve after treatment with portal decompression methods or liver transplantation. In addition to mosaic lesions, several studies have found that gastric erosions are also a form of BDDTAC. Gastric erosions are defects in the gastric mucosa with the bottom of the defect 0.3 - 0.5 cm in diameter. Some studies have shown that the frequency of gastric erosions is higher in cirrhotic patients than in non-cirrhotic patients. Some authors classify gastric erosions as a severe form of BDDTAC while others do not.
2. Frequency and natural course of portal hypertension
2.1 Frequency
Frequency of BDDTAC varies widely from 4-98% depending on the author. Research by Burak K.W. showed that the rate of BDDTAC in cirrhotic patients is 65%, of Primignani M. 80%, of Curvelo L.A. is 93.4%. In Vietnam, the study by Tran Ngoc Luu Phuong and CS has a rate of 42.6%, lower than most other studies abroad. Regarding the classification of BDDTAC, most studies show that the prevalence of mild BDDTAC ranges from 65-90% while severe BDDTAC accounts for 10 to 25%. However, some studies suggest that severe BDDTAC has a fairly high rate: The McCormack T.T. The rate of mild/severe BDDTAC was: 56.9%/43.1%, the study of Barakat M. was 68%/32%, of Curvelo L.A. is 48.8%/51.2%.
The explanation for this large variation is the difference between the study patient groups as well as the inconsistency among researchers in the definition and classification of BDDTAC.
2.2 Natural course of portal hypertension
Only a few studies have addressed the natural course of portal hypertension in cirrhotic patients.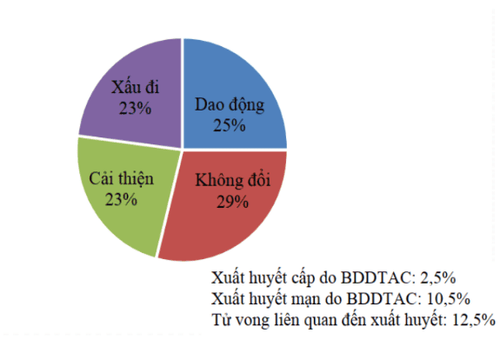
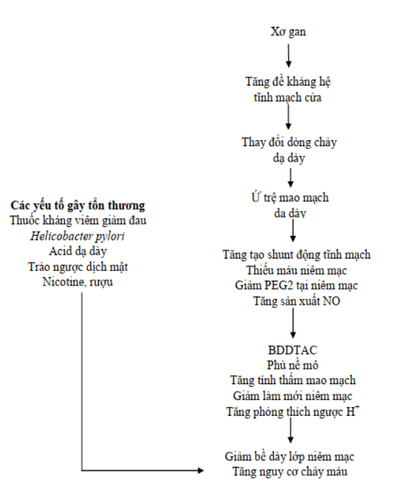
3. Pathogenesis of portal hypertension in patients with cirrhosis
3.1. Portal venous pressure
The most important factor in the formation of BDDTAC is portal hypertension. There is evidence that BDDTAC improves or may disappear with portal decompression treatments such as CBKCL drug therapy, TIPS placement, portal-host shunt surgery, or liver transplantation. In addition, BDDTAC is present even in patients with portal hypertension without cirrhosis. Some studies initially found an association between portal pressure and BDDTAC. Gupta R. found that the occurrence of BDDTAC was significantly more frequent in patients with esophageal varices than in patients without.
Some other studies show the opposite results. Sarin S.K. et al found that BDDTAC was associated with liver failure but not directly with varicose vein pressure.
3.2 Degree of liver failure
The influence of the degree of liver failure on the occurrence of BDDTAC remains controversial. Barakat M. found that severe BDDTAC occurred more frequently in patients with Child C grade than Child A, but it was not statistically significant. Dong L. found that there was a statistically significant relationship between the Child - Pugh grade and the occurrence and grade of BDDTAC (p < 0.05).
3.3. Flow factor
Gastric perfusion is also an important factor. Some studies have suggested that there is a decrease in gastric mucosal perfusion in BDDTAC while others have shown the opposite, some of which have shown no change.
Recent studies have shown an increase in gastric perfusion but with an uneven distribution in different regions: There is a relative decrease in perfusion in the mucosal region but an increase in the submucosal region. fascia, muscular layer, and serosa.
3.4. Disorders of humoral factors
Nitric Oxide (NO) is a potent vasodilator released from the endothelial cells of the vessel wall. Increased portal pressure acts on endothelial cells of the peripheral blood vessels to increase NO production, and conversely, NO causes vasodilation, increasing circulating flow, which in turn contributes to an increase in portal pressure. Research by Hartleb M. and El-Newihi H.M. showed an increase in serum NO in cirrhotic patients with BDDTAC and also an increase in NO synthesis in the gastric mucosa.However, administration of aminoguanidine (NO antagonist) to reduce circadian hyperactivity in rats with portal hypertension did not reduce BDDTAC progression. This suggests that NO contributes rather than determines the formation of BDDTAC. The role of prostaglandins in the formation of BDDTAC is still controversial. Studies in cirrhotic patients with BDDTAC of prostaglandins have produced contradictory results while animal studies have shown decreased prostaglandins. However, the use of prostaglandins inhibitors increases gastric damage in both humans and animals. Thus, there are several changes in humoral factors in BDDTAC formation. The most obvious change was an increase in NO concentration along with a disturbance of prostaglandins that increased the sensitivity of the gastric mucosa.
4.5. Decreased mucosal protective factor
In addition to the factors mentioned above, the factor that protects the gastric mucosa is also reduced. Agnihotri N. studied in rats with partial ligation of the portal vein showing BDDTAC.
Through observing gastric mucosal specimens and counting secretory cells on a microscope, the author found that there was a decrease in mucosal thickness along with a significant decrease in secretory cells and increased gastrin secretion. Quintero E. also found an increase in gastrin in cirrhotic patients with antral vasodilatation on histopathology with the appearance of red dot in the antrum.
Vinmec International General Hospital is a prestigious address trusted by many patients in performing diagnostic techniques for digestive diseases, hepatobiliary diseases, portal hypertension, cirrhosis... Along with At that time, at Vinmec Hospital, screening for gastric diseases was done through gastroscopy with Olympus CV 190 endoscope, with NBI (Narrow Banding Imaging) function for The imaging results of mucosal pathology analysis are clearer than conventional endoscopy, detecting atrophic gastritis lesions, intestinal metaplasia, low-grade, high-grade gastric dysplasia, and lesions. Inflammation and edema due to portal hypertension... Vinmec Hospital with modern facilities and equipment and a team of experienced specialists, always dedicated to medical examination and treatment, customers can peace of mind with gastroscopy and esophagoscopy services at Vinmec International General Hospital.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
References:
Nguyen Xuan Hien (2009), “Research on endoscopic images of esophageal mucosa in cirrhosis patients”, Vietnam Journal of Gastroenterology, p. 1075-1079. 2. Tran Van Huy, Pham Van Linh, Pham Minh Duc (2006), “Efficacy of endoscopic rubber band ligation in the treatment of bleeding due to ruptured esophageal varices”, Practical medicine, 532 , p. 23-29. 3. Tran Van Huy (2006), "Efficacy of endoscopic rubber band ligation combined with propranolol in preventing recurrence of esophageal varices rupture in patients with cirrhosis", Vietnamese Medicine, Hepatology. secret, p. 140-149 Study on the effectiveness of esophageal varices ligation in combination with propranolol in the prevention of recurrent bleeding and its impact on portal hypertension due to cirrhosis (2014). Tran Pham Chi, Doctor of Medicine Thesis, Hue University of Medicine and Pharmacy Nguyen Ngoc Thanh, Nguyen Thuy Oanh (2012), "Evaluate the effectiveness of methods to prevent recurrent esophageal varices rupture by elastic ligation combined with propranolol. , Journal of Medicine Ho Chi Minh City, 16 (3), p. 29-35.