This is an automatically translated article.
Portal hypertension can occur in many different diseases and is often difficult to detect until the disease causes complications. Treatment of portal hypertension is mainly surgical.
1. What is portal hypertension?
The portal vein is made up of 3 main veins, namely the splenic vein, superior mesenteric vein and inferior mesenteric vein, responsible for transporting blood from organs such as spleen, pancreas, stomach, intestines , colon to the liver.Portal hypertension is a condition in which the pressure in the portal vein is increased relative to the liver, when the hepatic venous pressure is > 5 mmHg.
2. Causes of portal hypertension
Bệnh nhân bị viêm gan B có thể là nguyên nhân gây tăng áp lực tĩnh mạch cửa
Causes of portal hypertension are classified as follows:
2.1 Pre-hepatic causes Portal vein thrombosis (due to liver cancer, cholangiocarcinoma, pancreatic cancer, stomach cancer or trauma), peritonitis, cholangitis, diverticulitis, appendicitis, acute pancreatitis, coagulopathy, ... cause); thrombosis of the splenic vein (caused by trauma, tumor, acute pancreatitis); External portal vein compression, cholangiocarcinoma, pancreatic tumor and metastasis of tumors.
2.2 Liver causes Cirrhosis (due to alcoholism or hepatitis B and C) is considered the main cause of portal hypertension. In addition, some other causes lead to cirrhosis such as autoimmune hepatitis, taking drugs that cause liver damage, primary and secondary biliary cirrhosis, primary biliary fibrosis, iron and copper deposition in liver tissue, hepatic venous obstruction, ...
2.3 Post-hepatic causes Right heart failure, constrictive pericarditis, Budd-Chiari hepatic veno-occlusive syndrome (due to acute coagulopathy, local or systemic inflammation) body, caused by chronic tumors).
3. Complications of portal hypertension
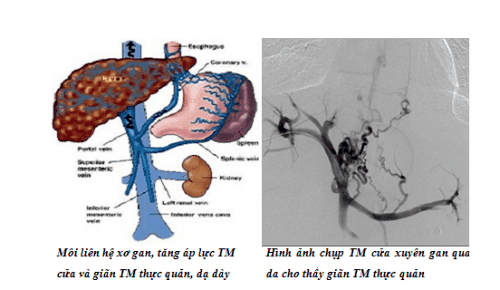
Giãn tĩnh mạch thực quản là biến chứng của tăng áp lực tĩnh mạch cửa
Increased portal pressure if left for a long time or is not detected and treated can cause complications such as:
Varicose veins of the esophagus, stomach, causing bleeding due to rupture of veins Enlarged spleen Ascites Inflammation peritonitis encephalopathy Hepatic encephalopathy Hepatobiliary syndrome Hepatocellular carcinoma
4. Symptoms of portal hypertension
Most portal hypertension does not have any symptoms until it causes the complications mentioned above. At that time, the patient was admitted to the hospital with symptoms such as:
Enlarged spleen: As a common symptom, the size of the spleen may increase to a degree of 4-5. Varicose veins of the abdominal wall: The veins in the abdominal wall from The navel to the chest to the groin are dilated, prominently on the subcutaneous surface, especially when sitting. Ascites: A symptom of severe portal hypertension. Gastrointestinal bleeding: The veins of the esophagus and stomach are dilated and ruptured, causing gastrointestinal bleeding, which can recur many times. Other manifestations: jaundice, leg edema, anemia, red palms.
5. Diagnosis of portal hypertension

Xét nghiệm máu chuẩn đoán chính xác tăng áp lực tĩnh mạch cửa
5.1 X-ray Contrast Esophageal X-ray: The results show that the esophageal veins are dilated into the lumen of the esophagus. Contrast-portal splenogram: The results allow to assess the extent to which portal hypertension causes portal vein dilation. Distal liver scan: Results show liver size. 5.2 Endoscopy Esophageal endoscopy: Endoscopy results allow to evaluate the degree of dilation of the esophageal veins, which is shown by the images of varicose veins that are pale blue, swollen and raised. In severe cases, bleeding in the esophagus may be seen due to rupture of esophageal veins or abrasion of the lining of the esophagus.
5.3 Ultrasound Abdominal ultrasound allows screening for cirrhosis causing portal hypertension with enlarged liver, altered liver surface, roughness, splenomegaly, and deformed liver tissue structure. Doppler ultrasound showed an abnormal portal vein flow wave pattern.
5.4 Blood tests Albumin and globulin levels: Decreased albumin and increased globulin levels are a sign of impaired liver function. Prothrombin ratio: A prothrombin ratio of 60-70% and a prolonged prothrombin time indicate hepatocellular impairment. Bilirubin, phosphatase ratio: An increased bilirubin and phosphatase ratio indicates impaired liver function due to portal hypertension. Ammonia levels: Increased ammonia levels indicate impaired liver function. Anemia: A decrease in the number of red blood cells, white blood cells, platelets and hematocrit is indicative of gastrointestinal anemia, folic acid deficiency in patients with alcoholic cirrhosis or splenomegaly. 5.5 Measurement of portal venous pressure Measurement of portal hypertension can be done by methods such as direct intraoperative portal puncture, indirect measurement of splenectomy, endoscopic venous pressure measurement. Esophageal catheterization, right cardiac catheterization measures pressure above the obturator and free liver.
5.6 Other methods
CT, MRI: Used when the ultrasound method does not give accurate results. CT and MRI can show the anatomy of the portal vein system. Liver biopsy : Used when ultrasound and other imaging techniques do not give accurate results. Liver biopsies are performed to assess the degree of cirrhosis.
6. Treatment of portal hypertension
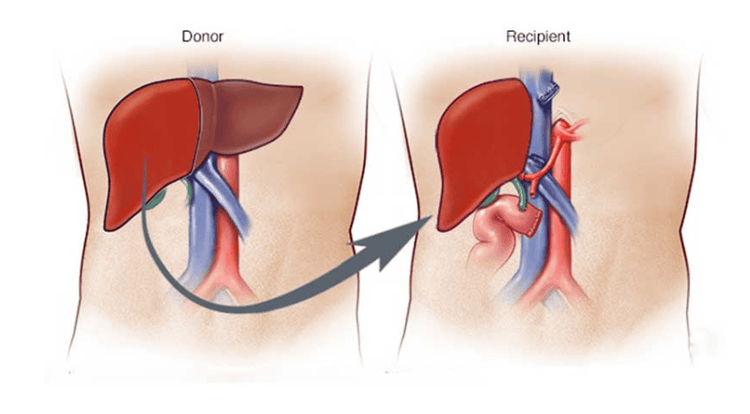
Phẫu thuật cấy ghép gan để điều trị tăng áp lực tĩnh mạch cửa
Portal hypertension is treated surgically including:
Treatment of portal hypertension Treatment of complications: Bleeding from ruptured esophageal varices, ascites Liver transplantation 6.1 Treatment of venous system decompression portal vein Treatment of portal venous system decompression can choose one of the following methods:
6.1.1. Surgical drainage of portal vein and vena cava system This method is indicated in cases of patients with marked portal hypertension, history of gastrointestinal bleeding and frequent recurrence, varicose veins. esophagus but liver function is still good; Contraindicated in cases of liver parenchymal damage, ascites. Surgery may choose to connect the portal vein to the vena cava; either the splenic vein to the peripheral/central renal vein, or the mesenteric vein to the vena cava. The advantage of the method is that it is highly effective in reducing venous pressure, causing less bleeding complications. However, the downside is that it can cause complications in liver or brain failure after surgery. 6.1.2. Surgery to create adhesions of the portal and host systems This method is performed with the aim of increasing lateral blood circulation, thereby reducing portal hypertension, indicated in cases where the patient does not have possibility or indications for venous anastomosis, contraindications for venous anastomosis due to liver dysfunction. Talma surgery (large omentum attached to the peritoneum or renal cavity), Nylander and Turunen surgery (lifting the spleen to the diaphragm by making an incision in the left diaphragm), Harman surgery (introducing the spleen into the abdominal wall) can be selected. . The advantage of this method is that it is light, but the pressure reduction efficiency of the door system is not high. 6.1.3. Surgery to reduce blood flow to the portal vein Splenectomy: Indicated in cases where splenic causes increase portal pressure. The surgical results allow a 30-40% reduction in blood volume and a decrease in portal pressure by 10cm of water. Splenic artery ligation surgery: The results of surgery help reduce portal pressure from 5 to 10cm of water. The advantages of this surgery are ease of use, maintenance of peri-splenic connections, and splenic pressure regulation. Liver artery ligation surgery: Indicated when cirrhosis causes portal hypertension. The result of surgery is to reduce blood volume in the sinuses, thereby reducing pressure in the portal vein. Vasectomy: The patient underwent splenectomy and the great curvature of the stomach, followed by ligation of 4 pedicles of the stomach including the coronary artery, the pylorus, the right omentum and the left gastric omentum. 6.2. Treatment of complications 6.2.1. Treatment of ruptured esophageal varices causing bleeding Increased portal pressure causes esophageal varices to dilate and cause bleeding complications. Medical treatment of hemostasis, if the patient does not respond, then surgical treatment with methods such as:
Surgical decompression of the portal vein. Direct surgical intervention for dilated esophageal veins, including: opening along the esophagus and hemostasis of varicose veins due to increased portal vein (Crile surgery); Ligation at both ends of dilated veins and 60% glucose injection (Boerama surgery). Surgery prevents blood flow between the portal system and the host system through the esophagus. Surgery to cut across or part of the fundus of the stomach and suture. Surgery to remove the lower 1/3 of the esophagus and part of the stomach below the cardia, then bring the intestine up and reconnect. Surgical resection of part of the esophagus above the cardia and below the cardia, followed by transplantation of a segment of small intestine with a feeding vessel. Surgical ligation of the esophagus above the cardia over the valve. 6.2.2. Treatment of ascites Treatment of multiple ascites is performed by surgical methods such as:
Surgical drainage of ascites water into the subcutaneous tissue Surgical drainage of ascites into the veins Surgery to drain the thoracic duct Bilateral adrenalectomy 6.3 Liver transplant surgery Liver transplantation allows radical treatment of portal hypertension. However, surgery and postoperative outcome depend on many factors such as liver source, immunological, biochemical, ...
Portal hypertension can cause many dangerous complications if not detected. and treatment.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.