This is an automatically translated article.
The article is professionally consulted by Master, Doctor Tong Van Hoan - Emergency Medicine Doctor - Emergency Department - Vinmec Danang International Hospital.Pneumothorax is a disease that needs immediate emergency care because it directly affects and affects respiratory function. Pneumothorax is easy to recognize due to its sudden onset with severe chest pain, dry cough, and shortness of breath.
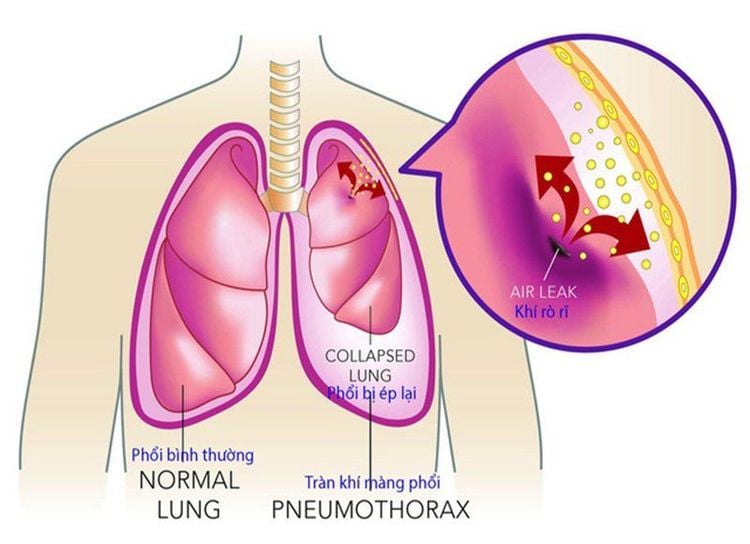
1. What is pneumothorax?
Pneumothorax is a condition in which air enters the pleural space (the space between the two pleural membranes) leading to atelectasis due to increased pleural pressure. Normal pleural pressure is from -3 to -5cm H2O, when there is pneumothorax, there is positive pressure from 10-25cm H2O.Air can enter the pleural space by 1 of 3 ways:
Through the airways, from the alveoli into the pleural space due to tearing of the visceral pleura Through the diaphragm, chest wall, mediastinum, or esophagus (in penetrating wounds) chest) Due to the existence of gas-producing microorganisms in the pleural cavity
2. Symptoms of pneumothorax
2.1. Physical and systemic symptoms The disease has a sudden onset, with severe chest pain. Shortness of breath feeling suffocated, the degree of dyspnea depends on the amount of air in the pleural space and previous lung disease. The patient may also have a dry cough. Systemic manifestations may or may not be fever. If the pneumothorax is severe, the patient may develop severe dyspnea, tachypnea, tachycardia, hypotension, and most seriously, cardiovascular collapse, cardiac arrest leading to death. 2.2. Physical Symptoms Major Pneumothorax:Pneumothorax dilated and reduced breathing movement Galliard's Triad: Percussion, reduced or absent pulsation, decreased or absent alveolar murmurs Cylindrical syndrome: Crumpled lung sounds as if blowing into a jar; voice and cough on auscultation of the lungs are high-pitched like talking and coughing into a metal vessel Low volume pneumothorax:
Physical symptoms are usually only reduced alveolar murmurs Combined pneumothorax may be seen: due to bleeding complications in the pleural cavity usually only 200-300ml of blood, if there is a lot of blood, think about rupture of the apical ligament of the lung.

Tràn khí màng phổi nặng có thể khiến bệnh nhân trụy tim mạch
3. Diagnosis of pneumothorax
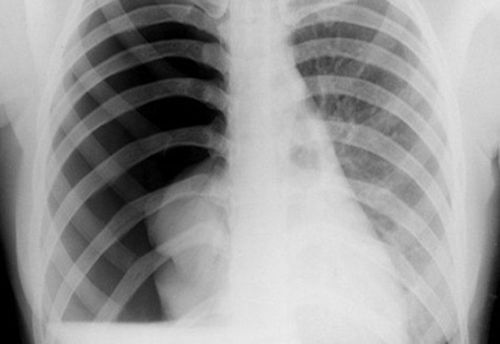
Diagnosis is made based on a combination of symptoms and laboratory tests. Some commonly used tests, including:X-ray:
In the case of small pneumothorax, an exhalation X-ray will show the image of a pneumothorax. Pneumothorax is characterized by increased light without striations in the lungs, the lungs are smaller than normal, the pleural-visceral contour is clearly seen, the intercostal space is dilated, and the heart, mediastinum, and diaphragm are lowered.
In case of effusion combined with pneumothorax, through X-ray, the water level in the pleura can be observed, combined with clinical examination, there is a yawning sound, a crackling sound.
CT scan:
If computed tomography is taken at the time when the lung is still collapsed due to compression of the air, the damage to the lung parenchyma will not be seen, so computed tomography should only be done after had aspiration or drainage of the pleural space. This method allows to record the cross-sectional view of the lung tissue. Based on the different density between healthy lung tissue, diseased part (bubble, tuberculous lesion, abscess, tumor, bronchiectasis, thickening) that we can determine quite accurately the Details of: location, extent of injury, degree of compression of the lung, mediastinum, and images on computed tomography also suggest us in determining the cause of pneumothorax. lung.
4. Treatment
4.1. Principle of treatment:Remove all pneumothorax, help the lung parenchyma expand close to the parietal pleura. Preventing the risk of recurrent VAP. 4.2. Remove all pneumothorax:
Just monitor:
Every day the body absorbs about 1.5% air on its own. To increase the time of gas absorption, give the patient more oxygen to breathe. Even in the absence of hypoxemia (the purpose is to increase the pressure gradient of nitrogen gas between the lungs and the pleural cavity), the nitrogen in the pleural cavity decreases, the rate of gas absorption will increase. Indicated for primary spontaneous pneumothorax, less pneumothorax < 20% of the volume on the side of the pneumothorax (peak < 3 cm, axillary < 2 cm), no need for drainage, Bed rest, Oxygen ventilation 2-3 liters/minute for 2-3 days, Can give more cough medicine, pain reliever. Then take chest X-ray to check, if stable, discharge from hospital. Simple pneumothorax:
- Indications:
❖ Young patient with primary spontaneous pneumothorax, symptomatic, high air volume > 20% of the volume in the pneumothorax.
❖ Pneumothorax secondary to procedures (pleural effusion, pleural biopsy, transthoracic lung biopsy), air volume < 15% of pneumothorax.
❖ Or is the first first aid operation to decompress the sphincter causing suffocation.
- Use a fine needle connected to the trimmer and the 50 mL syringe (electric pump type). After aspirating all the air, withdraw the needle. If 1 liter of air is aspirated but the air is still coming out evenly, there is no feeling that the air is about to run out, it is necessary to consider the indications for pleurodesis, or
- Use a catheter (14-16G) if connected to the infusion line, which tripod and 50 mL syringe. After aspirating all air, clamp the infusion line and lock the three-prong for 12 hours, after re-scan, if there is no recurrence of VAP, remove the catheter, or
- Insert a catheter with a polyethylene barrel into the pleural space:
❖ Suction with pressure - 20 cm of water continuously until the pneumothorax is gone, then clamp the drain for 24 hours.
❖ Remove the drain if there is no recurrence after 24 hours based on: clinical examination and chest X-ray.
❖ After clamping the tube, if the patient is found to have increased dyspnea and/or subcutaneous emphysema, open the clamp and re-aspirate immediately.
- Aspiration alone has a success rate of up to 50%.
Pleural drainage:
- Indications:
❖ Spontaneous (idiopathic), symptomatic primary pleural effusion, the first time, the amount is > 20%, after the needle aspiration failed.
❖ Pneumothorax positive pressure: breathing rate > 30 times/min, heart rate > 140 times/min, blood pressure drop. The mediastinum is pushed to the opposite side, the lower diaphragm is flattened and flat, sometimes reversed, subcutaneous emphysema. If the needle is inserted into the pleural cavity, a lot of gas will be seen.
❖ All cases of secondary spontaneous pulmonary embolism (pulmonary regurgitation in patients with COPD, pulmonary tuberculosis, lung abscess...).
TKMP due to trauma.
Pneumothorax secondary to artificial ventilation.
Pneumothorax combined with pleural effusion (because it may be associated with hemothorax).
- Proceed:
- Failure:
Air continues to come out after 5 days of continuous suctioning. Will invite a thoracic surgeon to consult and switch to surgical treatment.
5. Some types of pneumothorax
Tràn khí màng phổi tự phát thường xuất hiện đột ngột không rõ nguyên nhân
Open the pleura to aspirate closed drainage. Indications for pleural cavity endoscopy or surgery after failure of the above treatment measures. 5.2. Positive pressure PE:
As soon as it is detected, it is necessary to immediately remove the pneumothorax with a common needle or small catheter into the 2nd intercostal space about 1cm beyond the midclavicular line (to avoid damage to the internal mammary artery) or the intercostal space 4-5 middle axillary lines, to relieve pleural pressure. Open the pleura for early drainage. 5.3. Gastric bypass due to diagnostic and therapeutic procedures:
Post-procedural ventilation: low air volume requires fine-needle aspiration or placement of a pleural drainage tube. Open the pleura if there is a lot of air, fine-needle aspiration is not effective. Pneumothorax in patients with COPD due to balloon compression or mechanical ventilation, requires opening the pleural cavity with a 24-28F drain, followed by continuous aspiration and possibly sclerosing of the pleura with talc or pumped Iodopovidone. through the drain. Pneumothorax is a fairly common medical condition today with many different causes. Based on each cause, the doctor will give the best emergency treatment plan for pneumothorax for the patient.
Master. Doctor Tong Van Hoan has 10 years of experience in the field of Emergency Resuscitation, is capable of performing difficult techniques in Emergency Resuscitation such as advanced mechanical ventilation, continuous and intermittent dialysis, plasma exchange. , difficult airway intervention, hemodynamic monitoring by PiCCO, advanced cardiopulmonary resuscitation (ACLS), emergency bedside ultrasound, echocardiography...
Customers can go directly to the Health system Vinmec nationwide for medical examination and treatment or contact the hotline here for the best support.