This is an automatically translated article.
The article is professionally consulted by Master, Doctor La Thi Thuy - Cardiovascular Center - Vinmec Central Park International General Hospital.Veins are blood vessels that carry blood from the organs back to the heart. They are still at risk of inflammation or damage when impacted, affecting the body's ability to move or sometimes endangering life.
1. What is phlebitis?
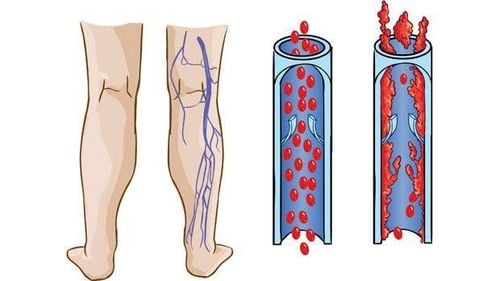
Peripheral vascular diseases are diseases of the blood vessels that do not nourish the heart, brain, and aorta. In other words, this is a group of diseases of the arteries, veins and lymphatic vessels that supply blood to the more distant organs such as the arms and legs. Phlebitis is also a common pathology in the group of peripheral vascular diseases.If the arteries are the blood vessels that carry blood from the heart to the organs in the body, providing oxygen and nutrients, then the veins are the way to return blood from the organs back to the heart. Phlebitis is thought to be when these blood vessels are damaged, structurally deformed, swollen, painful, or inflamed.
Depending on the characteristics of damaged veins, phlebitis is divided into two groups: superficial phlebitis and deep phlebitis.
Superficial veins are small in size, located shallowly under the skin and are visible to the naked eye. Phlebitis is often caused by external factors, such as intravenous catheterization for fluid infusion or drug infusion, hypertonic fluids. Superficial phlebitis may resolve spontaneously with discontinuation of therapy without specific treatment. Deep veins are larger in size, located deep inside the muscles of the legs and arms, and have valves to keep blood flowing one way back to the heart. Deep phlebitis is usually caused by the presence of a blood clot in the lumen of a vein and the condition is known as thrombophlebitis. At that time, it has the risk of moving to the lungs, causing unpredictable consequences if not timely intervention. It is important to recognize the risk factors and symptoms of the disease for early detection and early treatment.
2. What are the signs of phlebitis?

Viêm tĩnh mạch thường gặp ở chân.
Whether there is superficial or deep phlebitis, the patient will feel pain in the affected limb area, limited movement, the skin appears swollen, edematous, warm to the touch. beside.
Superficial phlebitis usually has a slow onset of a red, tender area along a vein in the skin. This area of skin may feel warm, painful, swollen, and itchy, with a burning sensation. Symptoms are worse with low legs, especially when getting out of bed in the morning. May be accompanied by a mild fever. If an infection is present, symptoms may include swelling, heat, redness, pain, fever, or skin lesions.
Deep phlebitis has symptoms similar to superficial phlebitis but some people have no symptoms. Some people experience pain and swelling of the entire lower extremity. The pain is more intense but difficult to pinpoint the exact location. If DVT is in the calf or thigh, the pain may be more noticeable when walking or flexing the leg.
Systemic symptoms often accompany cases of deep phlebitis. Patients with low-grade fever, fatigue or palpitations, rapid heart rate, shortness of breath, coughing up blood if the blood clot moves to the lungs, causing pulmonary embolism or infarction.
3. What causes phlebitis?
Phlebitis is most often caused by external influences, trauma or when the lining of the blood vessels is irritated.In the case of superficial phlebitis, the cause may be due to intravenous catheterization procedure, infected needle insertion site, injection of highly irritating drugs, highly concentrated intravenous fluids, etc.
In the case of deep vein thrombosis, the cause can also be the result of other conditions such as deep vein trauma due to surgery, fracture. If there is a prolonged lack of exercise, a long convalescence in bed after surgery or sitting after a long flight, a long standing position for many hours causes the venous system to dilate, stagnant blood flow also creates favorable conditions. thrombosis causing thrombophlebitis.
In addition, in some people, blood is also more likely to clot more easily than usual due to genetic diseases, imbalances between factors in the hemostasis system or possibly cancer. cancer, connective tissue disorder, autoimmune disease, oral contraceptive use or hormone therapy, pregnancy, overweight or obesity, smoking, alcoholism,...
4. Is phlebitis dangerous?
Superficial phlebitis is usually localized and does not lead to serious complications if triggers are promptly prevented. If left too late, aseptic superficial phlebitis will lead to an infection and when the infection spreads around it will cause a wound in the skin or even enter the bloodstream causing sepsis.For deep veinitis, in addition to the damage caused by local inflammation, the worrisome complication is when the blood clot moves through the blood vessels to the lungs, causing pulmonary embolism. If blood cannot reach the lungs, it will lead to a pulmonary infarction. If the volume of the necrotic lung area is large, the blood cannot receive oxygen from the outside, which can easily lead to respiratory failure, circulatory collapse and death. Therefore, deep vein thrombosis causing pulmonary embolism is a medical emergency requiring immediate treatment.
5. How to diagnose and treat phlebitis
The diagnosis of superficial phlebitis is usually simple, easily recognizable when the sources of influence are identified. The treatment only needs to remove the intravenous catheter, clean the wound if the cause is due to intravenous needle placement; Establish a central intravenous line when having to infuse hypertonic solutions, nutritional fluids, use anti-inflammatory drugs, etc. Since then, the inflammation, redness, swelling will quickly improve gradually. If an infection is suspected, or if there is a discharge of pus, the patient may need to be prescribed antibiotics for several days.For deep veinitis, in addition to the functional symptoms, risk factors, the disease may have to rely on tests, imaging to diagnose. The doctor will order an ultrasound of the blood vessels of the affected limb and the speed of the sound waves to help evaluate the flow rate, whether it is blocked or not; Sometimes thrombus can be observed, size and location can be described by ultrasound probe. If the possibility of pulmonary embolism cannot be ruled out, especially when the patient has symptoms such as dyspnea, respiratory failure, hemodynamic disturbances, contrast-enhanced computed tomography should be performed promptly. to check for the presence of a blood clot in the pulmonary artery.
The treatment of deep vein thrombosis is always complicated and the regimen is longer than that of superficial vein disease. Continuous anticoagulation therapy for three or six months and sometimes for life if the reason for thrombus formation is not fully resolved. For patients with contraindications to anticoagulation or experiencing drug-related complications, these cases need intervention to place a mesh filter on the vena cava to prevent blood clots from moving from the lower extremities to the lungs.
Patients with pulmonary embolism complications are also prescribed long-term anticoagulation. However, in emergency, life-threatening situations, thrombolytic drugs to dissolve blood clots require immediate indications or endovascular procedures to quickly remove the clot from the body.
6. How to prevent phlebitis?

Vận động sau phẫu thuật sớm giúp bệnh nhân nhanh hồi phục
Re-exercise as soon as possible after surgery, even passive movement in bed. Avoid standing for a long time in one position. Should wear compression stockings if the job requires a lot of walking. Regularly stand up, take a few steps or stretch your legs in place and drink plenty of water while sitting on a long flight. Vinmec International General Hospital treats phlebitis for patients with a scientific treatment regimen with the support of modern equipment. Hybrid operating room is equipped with advanced equipment such as DSA angiography machine, anesthesia machine with the most closely integrated patient hemodynamic monitoring software (PiCCO system, entropy,...). Therefore, the Hybrid operating room can meet the requirements of surgery and angioplasty, coronary stenting, aortic stent graft, open heart surgery, heart valve replacement for congenital heart diseases with modern minimally invasive techniques. most invasive, safe, help patients recover health soon.
Team of highly qualified cardiologists who have been trained and certified to perform the technique.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.