This is an automatically translated article.
The article was written by Specialist Doctor II Nguyen Thi Hoai Nam - Head of Pain Relief Unit - Department of Surgical Anesthesia - Vinmec Central Park International General Hospital
PPNI can lead to dysesthesia (sensory loss, hypoesthesia, hyperesthesia, paresthesia, and pain in areas innervated by the affected nerves) and/or motor impairment ( mild paralysis or even paralysis of the affected muscles). Autonomic dysfunction and nutritional changes can result in severe neuropathic pain.
1. Clinical Manifestations of Peripheral Nerve Injury (PPNI)
Evidence suggests that upper extremity nerve injury occurs more commonly than lower extremity injury (60/40). Symptoms and signs depend on the specific nerve affected. Manifestations of PPNI may occur only 48 hours after surgery, so the cause of the lesion may be suspected.
1.1 Injury to the peripheral nerves of the upper extremities 1.1.1 Injury to the ulnar nerve (C7,8 - T1) The shallow nature and close proximity to the medial condyle make the ulnar nerve most susceptible to perioperative injury. Three times more common in men, suggesting an anatomical predisposition that may play some role in this nerve damage (males have larger condyles and less protective fatty tissue that protects the nerve).
Often patients have subclinical neuropathy, which becomes exaggerated in the postoperative period. This was demonstrated by finding abnormal nerve conduction patterns (NCSs) in the contralateral arm. The mean age is 50 years and symptoms can be delayed up to 28 days after surgery.
Mechanism of injury: Direct compression of the ulnar groove at the elbow and prolonged flexion of the forearm are considered to be the most common causes of injury. In some cases, damage can occur, although the elbow is encapsulated as a result of subclinical damage to the already damaged nerve. Clinical Manifestations: Usually characterized by pruritus or numbness along the little finger and weak flexor or both. Examination of the hand revealed excessive extension of the metaphyseal joints and flexion at the proximal and distal interphalangeal joints of the ring and little fingers (ulnar claw). 1.1.2 Injury to brachial plexus (C5-T1): frequency 0.2-0.6% Favorable factors: shallow plexus, running between two fixed points (disc and axillary capsule), and its passage through a limited space between the collarbone and first rib and its proximity to some mobile bony structure that makes it vulnerable to injury. Mechanism of injury: Due to compression, stretching or direct trauma caused by regional anesthesia technique. Clavicle compression can occur during suturing of a midsternal cut or in a bilateral concave position with compression of the thorax and humerus head. Arm abduction, lateral shoulder rotation posteriorly, causes significant stretching of the roots on the brachial plexus. Similar results are seen when the arm is overexposed (>90°).
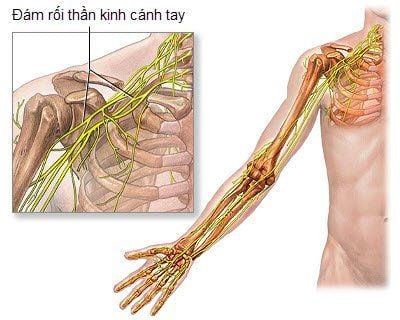
Clinical Manifestations : High damage to the C5–6 nerve root affecting the dermal, axillary and supraclavicular nerves, the arm is drooped to the side, internally rotated and prolapsed known as 'Waiter's Tip' . C8-T1 lesions mainly affect the small muscles of the hand, leading to hand grip and numbness in the ulnar nerve. 1.1.3 Injury to the radial nerve (C5-T1) Favorable factors : Coming from the posterior cord, the radial nerve running along the torsion groove of the humerus is the most commonly injured place. Mechanism of injury: Arterial sphygmomanometer cuffs/bands, compression on the patient or arm panels placed at incorrect height creating a step are the perioperative reasons thought to cause this nerve damage. Clinical Manifestations : Typically presents with wrist droop and numbness along the back of the lower arm, the back of the forearm, and a small variable area on the back of the hand and the outer three and a half fingers. 1.1.4 Injury to the median nerve (C5-T1) Mechanism of injury: Direct nerve damage caused by regional anesthetic techniques, invasive procedures around the elbow, and compression in the carpal tunnel are usually cause of this nerve damage.
Damage to the median nerve causing paresthesia of the palmar side of the three and a half lateral fingers. Motor manifestations include: weakness of the abductor and antithumb, weak flexion of the wrist, and supination of the forearm. The muscles of the hand tissue atrophy, the hand appears flat.
1.1.5 Injury to axillary nerve (C5,6) and musculoskeletal muscle (C5-7) These injuries are mainly caused by shoulder surgery or shoulder dislocation. Injury to the axillary nerve causes weakness of the shoulder and loss of sensation in the upper lateral arm, while weakness of the elbow flexors and lateral numbness of the lower leg are associated with neuromuscular injury.
1.2 Injury to the peripheral nerves of the lower extremities 1.2.1 Injury to the sciatic nerve (L4-S3) Mechanism of injury: Tension, compression, ischemia and direct injury are the main mechanisms. The obstetric, frog-leg, and sitting positions are associated with perioperative sciatica (excessive hip flexion, flexion and extension of the leg causing stretch). Regional anesthesia techniques and hip replacements can also cause injury. The incidence of lesions is higher in men aged 45–55 years and in patients with diabetes. The common peroneal nerve is also more commonly affected by lying more superficially than the tibial nerve. Clinical manifestations: paralysis of the hamstring muscles and all muscles below the knee leading to weak knee flexion and drooping foot. Decreased sensation below the knee except on the medial side of the lower leg and foot. 1.2.2 Injury to the femoral nerve (L2-4) Mechanism of injury: The femoral nerve can be injured by compression of the pelvic rim by the incision balls such as in abdominal-pelvic surgery, ischemia associated with transverse aortic clamping and obstetric posture with excessive femoral abduction and external rotation of the groin. It also involves invasive procedures to access the femoral blood vessels and hip replacement. Clinical manifestations: Loss of sensation in the front of the thigh and the medial side of the lower leg (sagittal nerve). Weak hip flexion and loss of knee extension make it difficult to climb stairs. Decrease or loss of the knee jerk reflex confirms the diagnosis.

1.3 Injury to the superficial peroneal nerve (L4-5, S1-2) Frequency of 0.88% in 2600 total knee replacements mainly due to surgical factors was noted.
Mechanism of injury: Obstetric posture and lateral position are common risk factors because nerves can be compressed at the fibula head. Long-term obstetric position was not associated with an increased risk of developing PPNI.
2. Diagnosis of Peripheral Nerve Injury (PPNI)
A thorough history and physical examination are necessary to locate the lesion and identify pre-existing peripheral neuropathy. Clinical examination to determine whether single or multiple nerve involvement and severity of motor, sensory, or both impairment is of prognostic value. If a defect is found, electrophysiological and imaging studies are performed and early consultation with a neurologist is required.
2.1 Electrophysiology and nerve conduction Electromyography (EMG) involves recording reproduces the electrical activity of a muscle at rest and during movement from a needle electrode inserted into it. The presence and nature of abnormalities depends on the affected composition of the motor unit, with the distribution of abnormalities suggesting a possible origin of the lesion.
Decrease in the number of active axons, which is pathophysiological in most PPNIs, leads to a decrease in the number of mobilized motor units. Abnormal spontaneous activity (vibration potential; chromophore due to impaired muscle tone) takes 1–4 weeks to develop and disappears after nerve redistribution. Their presence early suggests a pre-existing condition and a specific etiological diagnosis cannot be made.
Neurotransmissions (NCSs) allow assessment of motor and sensory nerve function. The conduction velocity and size of the muscle response estimate the number of activated axons and muscle fibers. NCSs assess the functional integrity of peripheral nerves and allow localization of lesions. Complex sensory action potentials will be reduced in axonal degeneration if the electrodes press on the affected part of the nerve.
During demyelination, there is a focal slowing of sensory or sensory and motor conduction across the injured part of the nerve (proportional to the severity of the demyelination) . NCSs may suggest the presence of a subclinical neuropathy leading to nerve damage and may also suggest the underlying pathological process (axonal loss versus demyelination), significance for clinical course and prognosis.
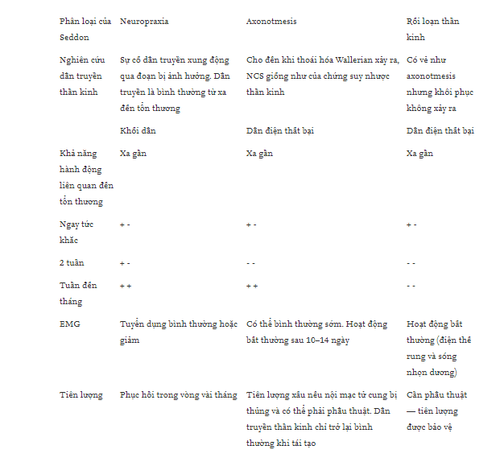
NCSs and EMGs complement each other and can help determine if the lesion is complete or incomplete; determine the basis of the clinical defect; localized lesions; determine the severity and age of the lesion; and guide prognosis and recovery. Table 2 illustrates the results of EMGs and NCSs performed in different lesions at different time points and lesion prognosis.
2.2 Imaging exploration 3.0 tesla magnetic resonance imaging provides adequate resolution for visualization of peripheral nerves and can be used to recognize and locate lesions, particularly if the site cannot be determined by electrophysiological testing. High-resolution ultrasound has also been proposed as an adjunct to electrical diagnosis.
3. Prevention of PPNI
American Society of Anesthesiology has noted in its practice to prevent PPNIs. Having a good knowledge of the anatomy and the risks associated with positioning the patient for surgery is essential for understanding prevention strategies. There is little evidence for recommendations, largely based on empirical knowledge and consensus.
A thorough history and preoperative examination are important to determine if the patient may have prior neurological damage and dysfunction. Intraoperative hypotension, hypothermia and dehydration should be avoided. Careful positioning of the patient, protective padding, arm padding, and avoidance of contact with hard surfaces or supports that can put direct pressure on sensitive peripheral nerves are important components of the perioperative care.
Arm extension should be limited to < 90 degrees in the supine position to prevent damage to the brachial plexus. Protection of the ulnar and median nerve: must have padding and forearm in supine or intermediate position. Bend and extend elbows should be ≤ 90 degrees. Measures to prevent nerve damage in the lower extremities include padding that is suitable for the patient in the obstetric, prone, and supine positions with hip flexion ≤ 120 degrees. Appropriate procedures should be in place when prescribing particular patient positions and particular care should be taken in areas of poor practice. A simple assessment of postoperative neurological function can detect peripheral nerve damage early.
No nerve tracking or localization technique has been shown to be clearly superior in reducing the frequency of clinical lesions in regional anaesthesia. Consideration should be given to avoiding stronger local anesthetics (ropivacaine is considered the least toxic) and vasopressors in patients with pre-existing neurological disease or peripheral nerve damage. Pain or paresthesia on injection may suggest injecting perineurium and the needle should be withdrawn or anaesthesia should be discontinued.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.