This is an automatically translated article.
The article was written by Specialist Doctor II Nguyen Thi Hoai Nam - Head of Pain Relief Unit - Department of Surgical Anesthesia - Vinmec Central Park International General Hospital1. Learn about Perioperative Peripheral Nerve Injury (PPNI)
PPNI is a complication of general and regional anesthesia. Two closed analyzes by ASA (American Society of Anesthesiology) over 10 years revealed anesthesia-associated nerve damage (28% ulnar nerve, 20% brachial plexus, lumbar nerve root). along with 16% and spinal cord 13%) accounted for 15% and 16% of all complaints respectively.
It is difficult to accurately determine PPNI rates due to the quality and heterogeneity of studies. A retrospective study found the PPNI rate to be 0.14% in general surgery if patients with axial or peripheral nerve anesthesia were excluded, whereas if these patients were not excluded the rate was 0. 11%. A retrospective study in the general surgical population showed a PPNI rate of 0.03% (112/380680 patients). Cylindrical neuropathy accounted for 0.037%, lower extremity neuropathy in obstetric position was 0.028%-1.5%.

2. Mechanism of perioperative peripheral nerve damage
Mechanisms of injury include compression, ischemia from stretching, direct nerve injury, and anesthetic toxicity. Classification of injury mechanisms and predisposing factors:Direct nerve damage: Due to surgery, needle trauma secondary to regional anesthesia or peripheral nerve catheter. The blunt needle is less able to penetrate the perineurium layer of the nerve, so it causes less damage. Due to tension and compression : Poor padding and patient posture, using tourniquets, opening the incision ischemic ischemia : This is often the most common final pathway of nerve damage and is mainly caused by tourniquet, prolonged immobilization, peri-nerve hematoma, and anesthetic agents. Toxicity of local anesthetics: Local anesthetics can cause cytotoxic axonal damage, especially if the solution is injected within the nerve fiber. High concentrations of local anesthetics and prolonged exposure can lead to nerve damage.

Double compression syndrome: a compression injury occurs along a nerve that makes the nerve less resistant to compression in the same or second location. Therefore, pre-existing nerve damage or compression (eg, patients with diabetes or patients with rheumatoid arthritis with unstable joints) are at higher risk for secondary damage, It is possible that subclinical damage leads to permanent neurological damage. Surgical factors: Neurosurgery, cardiac surgery, gastrointestinal surgery, and orthopedic surgery are associated with a higher incidence of PPNI. Patient factors: Hypertension, diabetes, and smoking induce microvascular changes that may make these patients more susceptible to PPNI. Double compression syndrome due to altered neuronal homeostasis may also play a role in these patients. Pre-existing peripheral neuropathy may predispose to PPNI. Anatomical abnormalities, particularly of the thoracic outlet and the elbow, can also predispose patients to PPNI. Anesthesia factor: General anesthesia and epidural anesthesia are associated with a higher incidence of PPNI than in sedated patients, where the patient can change position during surgery. Perioperative factors: Hypovolemia, dehydration, hypotension, hypoxemia, electrolyte disturbances, and hypothermia are associated with progression of PPNI
3. Classification of nerve damage
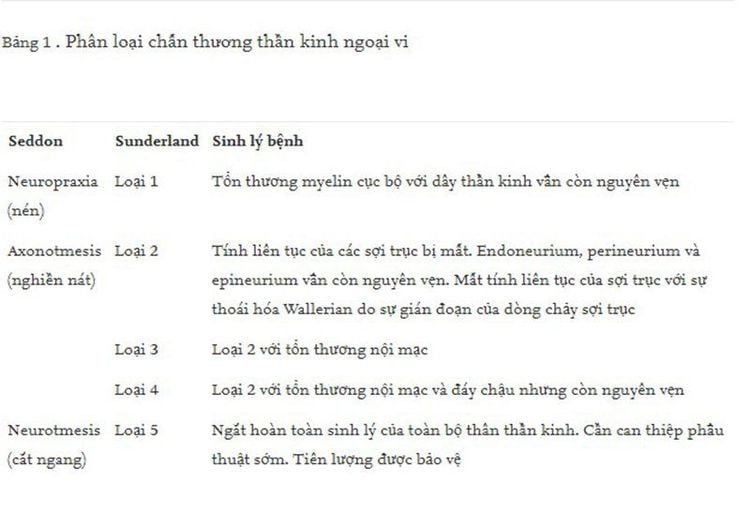
The most widely accepted classification of nerve damage are those described by Seddon (neuropraxia, axonotmesis and neurotmesis) and by Sunderland (nerve damage grades 1-5). The pathophysiological features are described in Table 1.
With many years of experience in the examination and treatment of neurological diseases, Vinmec International General Hospital has now become one of the major health care centers, capable of examining and screening. and treat many specialized diseases. Therefore, if there are signs of peripheral nerve damage, patients can go to Vinmec International General Hospital to examine and receive support and advice from doctors.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.