This is an automatically translated article.
Post by Master, Doctor Mai Vien Phuong - Department of Examination & Internal Medicine - Vinmec Central Park International General Hospital
Periodontitis is a chronic infectious and inflammatory disease of the periodontal tissues caused by the interaction between the microflora in the canal and the host immune system. The destruction of periodontal tissues can induce the activation of a variety of cytokines involved in the pathophysiology of ulcerative colitis. In addition, changes in the gut microbiota and immunosuppressive agents used to treat enteritis may worsen oral health through changes in the oral microbiota, lead to increased risk for periodontal disease. Periodontitis and inflammatory bowel disease are characterized by chronic inflammation that begins in the intestinal tract and shares some similar pathophysiological features. However, the pathogenic relationship between periodontitis and inflammatory bowel disease remains unclear. Epidemiological studies regarding the influence of periodontitis based on age and environmental factors on the occurrence of IBD are lacking.
1. Periodontitis is closely related to the pathogenesis of systemic diseases
Inflammatory bowel diseases (IBD), including Crohn's disease and ulcerative colitis, are chronic recurrent inflammatory diseases of the gastrointestinal tract with multiple etiologies. Complex interactions between dysbiosis, changes in the host immune system, and genetic factors influence the development of IBD. In Asia, the prevalence of IBD is increasing rapidly, and its genetic predisposition and environmental impact are different from those of Western countries. Environmental factors such as smoking and alcohol consumption may be involved in the development of IBD. The effect of smoking on the pathogenesis of Crohn's disease and ulcerative colitis is different. Smoking may have a small role in the development of Crohn's disease in Asia, unlike Western populations. In contrast, former smokers have a significantly higher risk of developing ulcerative colitis than non-smokers. Drinking alcohol is associated with worsening of symptoms in IBD patients.2. What do the studies say?
A nationwide population-based cohort study that was conducted in Korea on 9950548 people aged 20 years and older who underwent the national health examination in 2009 was included. Newly diagnosed IBD [Crohn's disease, ulcerative colitis] using the 10th International Classification of Diseases and the Rare Disease Code, compared between periodontitis and non-periodontitis as of 2017 A total of 1092825 people (11.0%) had periodontitis. Periodontitis was significantly associated with older age, male sex, higher body mass index, quitting smoking, not drinking alcohol, and regular exercise. The mean age was 51.4 ± 12.9 years old in the periodontitis group and 46.6 ± 14.2 years in the non-periodontitis group, respectively (P < 0.01). Median follow-up was 7.26 years. People with periodontitis had a significantly higher risk of ulcerative colitis than those without periodontitis [adjusted hazard ratio: 1,091; 95% CI: 1.008-1.182], but not Crohn's disease (adjusted hazard ratio: 0.879; 95% CI: 0.731-1.057). The risk for ulcerative colitis was significant in the subgroups of age ≥65 years, male sex, drinkers, current smokers, and reduced physical activity. Current smokers over the age of 65 with periodontitis have a 1.9-fold increased risk of ulcerative colitis compared with non-smokers over the age of 65 without periodontitis. Authors' conclusions from this study: Periodontitis is significantly associated with the risk of developing ulcerative colitis, but not Crohn's disease, particularly in current smokers over age 65.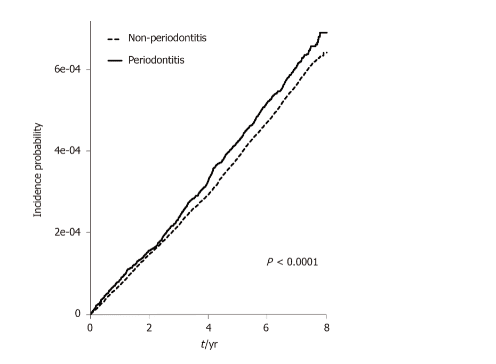
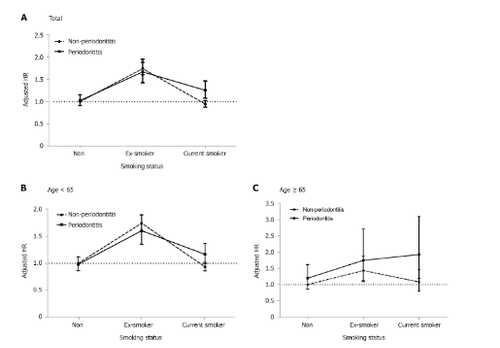
Risks of developing ulcerative colitis according to smoking behavior
The authors investigated the risks of developing ulcerative colitis in the periodontitis and non-periodontitis groups, according to smoking behaviour. Former smokers in both groups had the highest risk of developing ulcerative colitis compared with non-smokers with periodontitis, but the difference in adjusted rates between the periodontitis groups (HR adjusted: 1.667; 95% CI: 1.425-1,950) and non-periodontitis group (adjusted HR: 1,740; 95% CI: 1.606-1,884) in former smokers was not significant. However, current smokers in the periodontitis group (adjusted HR: 1.255; 95% CI: 1.078-1.462) had a significantly higher risk of developing ulcerative colitis, but not those in the group. without periodontitis (adjusted HR: 0.946; 95% CI: 0.874–1.025) compared with non-smokers without periodontitis. A significant difference in adjusted heart rate was observed between the periodontitis and non-periodontitis group in current smokers (Figure 3A). The risk of developing significant ulcerative colitis in current smokers with periodontitis (adjusted HR: 1,924; 95% CI: 1.197–3,092) was more pronounced in the elderly >65 years than in those with Non-smoker does not have periodontitis.
Studies show periodontitis significantly increases the risk of developing ulcerative colitis
This population-based cohort study of about 10 million people reported that periodontitis significantly increases the risk of developing it. ulcerative colitis, but not Crohn's disease, compared with those without periodontitis. The effect of periodontitis on the risk of developing ulcerative colitis is prominent, especially in elderly men who smoke, drink alcohol, and engage in reduced physical activity. In particular, current smoking and the presence of periodontal disease have a synergistic effect on the occurrence of ulcerative colitis in the elderly. To the best of our knowledge, this is the largest epidemiological study demonstrating the impact of periodontitis on the development of IBD based on demographic and environmental factors. In contrast, there is little evidence regarding the risk of developing IBD in periodontitis patients
A Taiwanese cohort study reported a higher risk of ulcerative colitis, but not Crohn's disease, A significant 1.56-fold in 27,000 patients with periodontal disease, including acute periodontitis, chronic periodontitis, and gingivitis, comparable to the authors' results in a nationwide study over 1 million subjects had chronic periodontitis. The authors' study has the strength of demonstrating the impact of chronic periodontitis, which may reflect the dynamics of chronic inflammatory conditions and lifestyle factors, such as smoking, on pathogenesis of IBD. Taken together, the risk of developing ulcerative colitis was significantly increased in patients with periodontitis, although the relatively low HR for ulcerative colitis in the periodontitis group should be assessed by epidemiological studies. epidemiology in other countries. Cause of this association
The role of the gut microbiota is crucial in the pathogenesis of IBD in terms of nutrition, host immune response, and defence. Ulcerative colitis is associated with reduced microbial diversity and depletion of Bacteroidetes and Firmicutes in the gastrointestinal tract. Disturbance in gut microbiota in IBD, particularly ulcerative colitis, is associated with changes in the salivary microbiome. Thus, oral hygiene and periodontal biofilm may influence the initiation and permanence of dysbacteriosis in the colon. In contrast, the dynamic interactions between the oral microbiome and the development of enteritis in patients with Crohn's disease are very weak. In a recent population-based cohort study in Sweden, dental plaque was negatively associated with a 68% reduction in the risk of Crohn's disease. The dynamic effects of oral hygiene on dysbiosis and chronic inflammation in the gastrointestinal tract need to be elucidated in further studies. Conclusion
The effect of periodontitis on the risk of developing ulcerative colitis is prominent, especially in elderly men who smoke, drink alcohol, and engage in reduced physical activity. In particular, current smoking and the presence of periodontal disease have a synergistic effect on the occurrence of ulcerative colitis in the elderly. Periodontitis and inflammatory bowel disease are characterized by chronic inflammation that begins in the intestinal tract and shares some similar pathophysiological features. However, the pathogenic relationship between periodontitis and inflammatory bowel disease remains unclear.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.