This is an automatically translated article.
The article is made by Master, Doctor Ton Nu Tra My - Department of Diagnostic Imaging - Vinmec Central Park International General Hospital.
Pelvic magnetic resonance imaging with injection of magnetic contrast is a widely applied method in the diagnosis of pelvic diseases because of its advantages of high accuracy, safety and low risk of complications.
1. Why is it necessary to have a pelvic magnetic resonance imaging (MRI) scan with magnetic contrast injection?
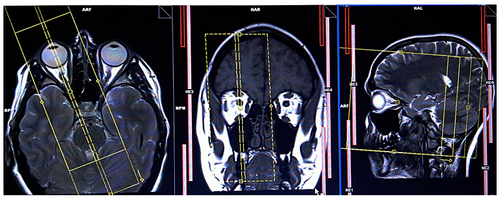
Magnetic resonance imaging is an advanced imaging method, which is a tomography technique that uses magnetic waves and radio waves. When taking magnetic resonance imaging, the hydrogen atoms in the body will be absorbed, releasing RF energy. The machine will receive the release process, process and convert the received signals into images.
High-quality, high-contrast, sharp, detailed and clear magnetic resonance imaging images, capable of 3D reconstruction and good anatomy, making it easy for doctors to accurately diagnose diseases core.
Magnetic resonance imaging is applied in the diagnosis of many diseases on the body in general, pelvic pathology in particular. Usually, magnetic resonance imaging without injection of magnetic contrast (gadolinium) is sufficient to confirm the diagnosis of many diseases. However, in some cases where a higher degree of tissue discrimination is required, and the blood supply of the lesion needs to be assessed, the doctor will assign the patient to have a pelvic magnetic resonance imaging (MRI) scan with injection of magnetic contrast agent.
2. Details of pelvic magnetic resonance imaging procedure with magnetic contrast injection
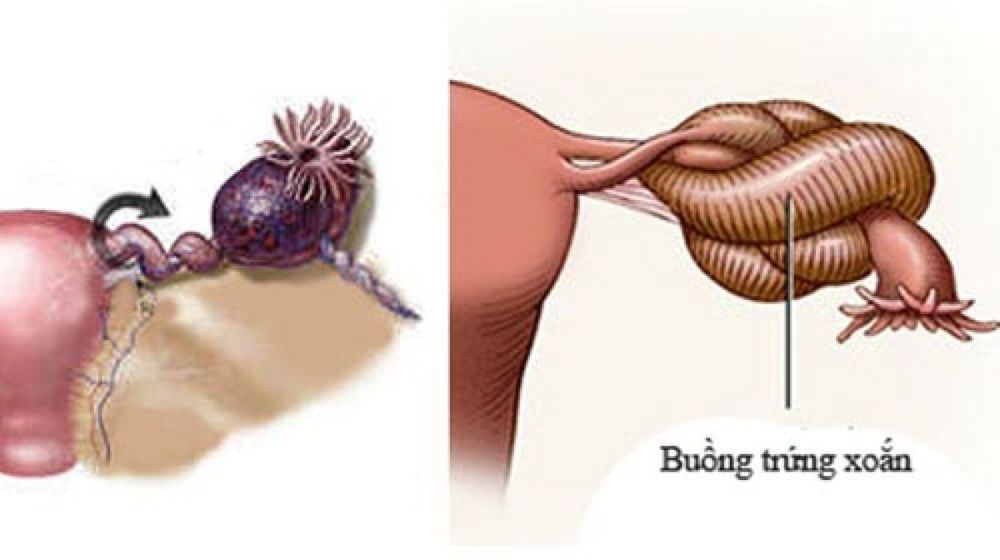
Chụp cộng hưởng chỉ định với trường hợp u nang buồng trứng xoắn
2.1 Indications Detection, staging of gynecological tumors of malignant nature, originating from the vulva, cervix, uterus, fallopian tubes and ovaries; Check to identify tumors or inflammation of the appendages with complications such as pus, ovarian cysts, fluid retention, ... or when the patient has pain due to suspicion of uterine leiomyoma, endometriosis ; Determine the number and location of uterine leiomyomas before surgical removal, uterine embolization or hysterectomy; Identify one or several congenital abnormalities in the pelvic organs of men and women; Evaluation of pelvic floor defects related to urinary or bowel incontinence; Detection and staging of malignancies in the rectum, bladder, prostate, penis and scrotum; Evaluation of complications after pelvic surgery, including urinary cysts, lymphatic cysts, abscesses, radiation enteritis, and fistula formation (especially anal fistula); Evaluation of tumor recurrence in the rectum, bladder, prostate or gynecological organs after surgical removal or dissection of the tumor; Identification and staging of sarcomas of tissue origin; Determine the anatomy - pelvic veins; Determining the cause of abdominal pain in pregnant women (including appendicitis or abnormal masses in the uterus and ovaries); Evaluation of fetal abnormalities in pregnant women.

máy chụp cộng hưởng từ
2.2 Contraindications Absolute contraindications:
Cases where patients wear electronic devices such as defibrillators, ear canal implants, pacemakers, automatic subcutaneous drug pumps, etc. .; Severe patients need to place resuscitation equipment close to the body; Patients with vascular, intracranial, or orbital metal surgical clips for less than 6 months. Relative contraindications:
Patients with metal surgical clips for more than 6 months; The patient is afraid of the closed or afraid of the dark. 2.3 Preparation before the MRI Operational staff: Specialist doctors, radiology technicians and nurses; Prepare the patient: The patient is thoroughly explained about the procedure to coordinate well with the doctor; no need to fast (must fast); checked for contraindications; be instructed to change clothes of the magnetic resonance imaging room, remove contraindicated items; have a written request for magnetic resonance imaging from a doctor or a complete medical record if necessary; Vehicles: Resonance machine of 1.5 Tesla or more; film, film printers and image storage systems; Medical supplies: 18G intravenous needle, 10ml syringe, gloves, cotton, gauze, sterile adhesive bandages, distilled water or physiological saline, medicine box, emergency equipment for contrast drug accidents; Drugs: Magnetic contrast agents, sedatives and skin and mucosal antiseptics.
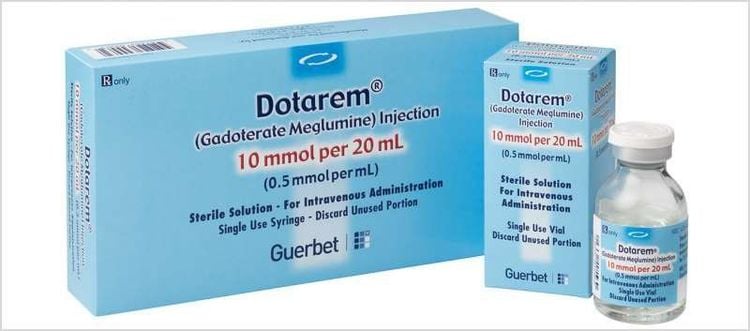
Thuốc đối quang từ
2.4 Procedure Patient position: Lie supine on the imaging table, footrest, using appropriate receiver coil available on the MRI machine, placing the patient's hand on the chest or on the head, options - locate the receiver coil, give the patient an emergency call button, move the table into the magnetic field of the MRI machine and locate the imaging area; The doctor placed an intravenous line with an 18G needle, connected to a double-bore injector (1 barrel containing physiological saline and 1 barrel containing magnetic contrast). The amount of contrast drug used is 0.1mmol/kg body weight; Location capture; Take before contrast injection: Take pulse sequences 1 - 2 - 3 - 4 according to the correct technique; Taken after injection of magnetic contrast; Perform magnetic contrast injection at a dose of 0.1mmol/kg body weight at a rate of 3ml/sec. The technician prints the film and transfers the image to the doctor's workstation; The doctor performs image analysis, evaluates the results. Note: Intravenous inotropic drugs can be used to reduce bowel movements for patients; The seat belt can be tied across the patient's abdomen to limit respiratory movement and remind the patient to breathe through the chest.
2.5 Some common complications Patient is scared and agitated: The doctor should encourage and comfort the patient; Patients are too worried, scared: Can give patients sedatives under the supervision of anesthesiologists; Contrast-related complications: Including conditions such as urticaria, nausea, anaphylaxis, hypotension, laryngeal edema, bronchospasm,... When experiencing these complications, the doctor Doctors need to treat according to the standard protocol (see also the section on anaphylaxis management protocol)

Bệnh nhân có thể bị tụt huyết áp khi chụp cộng hưởng từ vùng chậu có tiêm thuốc đối quang từ
Vinmec International General Hospital put into use the magnetic resonance imaging machine 3.0 Tesla Silent technology. Magnetic resonance imaging machine 3.0 Tesla with Silent technology of GE Healthcare (USA).
Silent technology is especially beneficial for patients who are children, the elderly, weak health patients and patients undergoing surgery. Limiting noise, creating comfort and reducing stress for customers during the shooting process, helping to capture better quality images and shorten the shooting time. Magnetic resonance imaging technology is the technology applied in the most popular and safest imaging method today because of its accuracy, non-invasiveness and non-X-ray use.
Master. Dr. Ton Nu Tra My is currently a Doctor of Radiology, Vinmec Central Park International General Hospital. Dr. Tra My used to be a lecturer in the Department of Diagnostic Imaging, Hue University of Medicine and Pharmacy and had a long time working at the Department of Diagnostic Imaging, Hue University of Medicine and Pharmacy Hospital.
To register for examination and treatment at Vinmec International General Hospital, customers can call Hotlines of hospitals or register online HERE.