This is an automatically translated article.
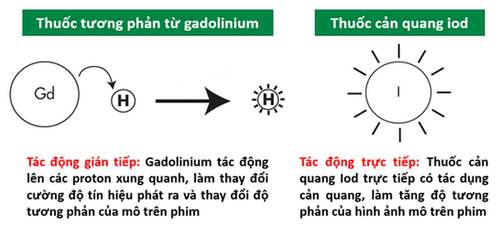
The article was written by MSc Nguyen Le Thao Tram - Doctor of Diagnostic Imaging, Department of Diagnostic Imaging - Vinmec Nha Trang International General Hospital.Contrast drug with "gadolinium" base, based on paramagnetic properties acting on protons of water molecules, containing Hydrogen (H) atom - is the basic element in magnetic resonance imaging technique, contributing to the part that alters the contrast of the examined tissue.
1. What is magnetic contrast drug?
Magnetic contrast (also known as magnetic contrast) was first approved in 1988 by the FDA, is an effective arm to help doctors make a better diagnosis based on image contrast in computed tomography. benefit from.
Magnetic contrast agent is not a contrast agent, not only because it does not contain the iodine component as in existing contrast agents, but also because of the nature of the mechanism of action on the cellular component.
2. Magnetic contrast agents used in magnetic resonance today?
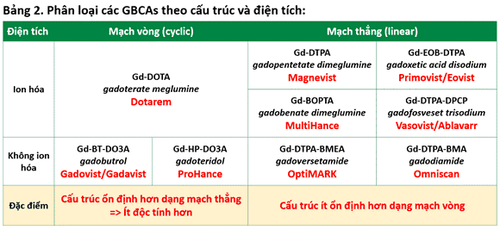
Currently, there are 7 types of Gadolinium-based contrast agents (Gd) that are widely used in the world. Since 2017, a number of linear ionic contrast agents have been restricted for use in Europe because of the risk of free gadolinium toxicity.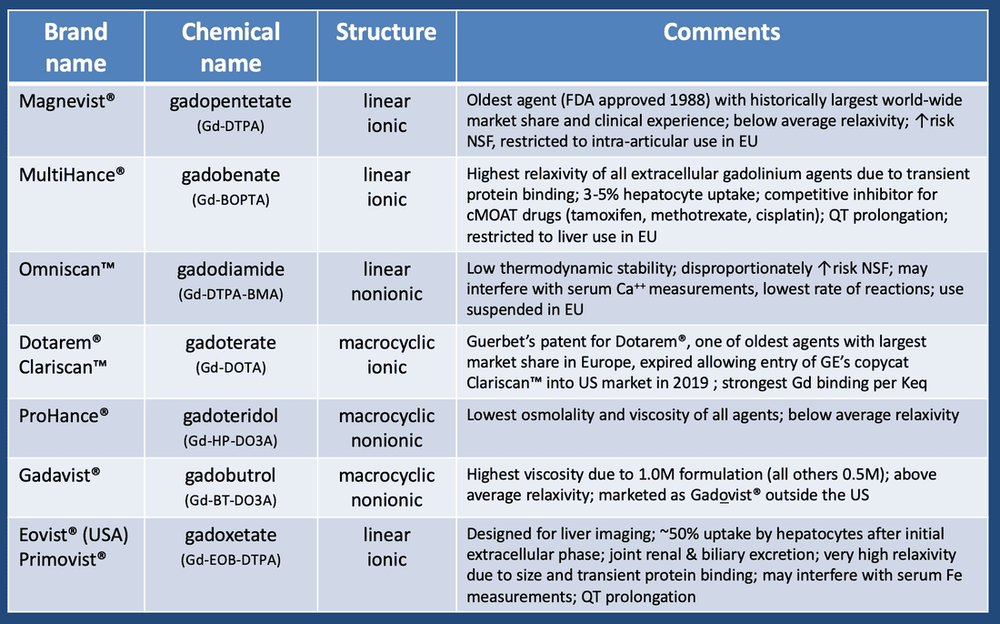
3. Effects and indications of magnetic contrast drugs?
Regarding the pharmacokinetic mechanism, the contrast agent enhances the contrast of the examined tissue. In other words, contrast agents help to increase the accuracy of imaging studies. The indication to use the drug is applied on a case-by-case basis, your doctors will notify you or your family if you need to use contrast agents. In general, the drug will help increase the ability to evaluate inflammatory lesions, tumors, vascular examination and perfusion properties of each organ.
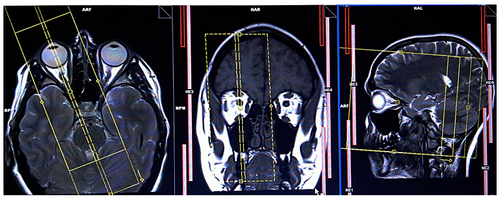
Magnetic contrast agents are used most effectively for the brain and spinal cord, because when the blood-brain barrier is pathologically damaged, the signal of the damage is markedly increased. In diseases such as arthritis, tumors, inflammation in solid organs, contrast agents are also valuable to evaluate lesions.
Using magnetic contrast is also significant in vascular survey (MRA technique - MR angiogram), based on the signal capture of the drug in the flow, to survey intracranial and extracranial blood vessels in different phases. arteries and veins.
4. Undesirable effects of magnetic contrast drugs?
Side effects from contrast agents are almost minimal. Since 1988, since they were approved by the FDA, contrast agents have been considered very safe to use. Life-threatening side effects within 24 hours are seen with a very low incidence of 0.001 - 0.01%. Manifestations recorded in the literature are mainly neurological reactions with headache, dizziness, vomiting, nausea, paresthesia, metallic taste in mouth, convulsions... and hypersensitivity reactions such as allergic reactions. Skin reactions , anaphylaxis ...
A very late side effect associated with gadolinium contrast agents may be renal systemic fibrosis (NSF). The onset of this condition can occur on the day of use up to 2-3 months later, sometimes even years later, and manifests as pain, severe itching, swelling, and erythema, usually starting in the legs. Later, late manifestations may include thickening and fibrosis of the skin and subcutaneous tissue, limb contractures, fibrosis of organs or even death if the damage to the organs is severe.

Người bệnh có thể gặp tình trạng ngứa và xuất hiện hồng ban sau khi dùng thuốc đối quang từ
Most of the reported cases of NSF were caused by gadodiamide (Omniscan) with a frequency of 3 - 18%, which may occur after gadopentetate dimeglumine (Magnevist, Multihance) at a rate of 0.1 - 1% and gadoversetamide (Optimmark, Primovist, Eovist), the risk increases with increasing dose. This disease is likely to occur in patients with reduced renal function (glomerular filtration rate <15ml/min/1.73m2 skin).
The risk of NSF was lowest with gadobutrol (Gadovist, Gadavist), gadoterate meglumine (Dotarem, Magnescope), gadoteridol (Prohance).
The risk of gadolinium deposition in the body can persist for several months to several years. Gadolinium concentrations were highest in bone, brain, skin, kidney, liver and spleen. In which the drugs Omniscan, Optimark have the highest risk of deposition, whereas Dotarem, Gadovist, Prohance have the lowest risk of deposition.
In the Drug Safety Bulletin of December 19, 2017, the FDA concluded that drug deposition was not directly related to adverse events in patients with normal renal function, and that the benefits of the drug outweighed potential hazard if appropriately indicated. However, if not absolutely necessary, clinicians will minimize the repeated use of contrast agents in two close-ups.
The above article uses materials of some colleagues, as well as references to documents from a number of specialized websites at home and abroad.
Customers can directly go to Vinmec Health system nationwide to visit or contact the hotline here for support.