This is an automatically translated article.
Post by Master, Doctor Mai Vien Phuong - Gastrointestinal Endoscopy - Department of Medical Examination & Internal Medicine - Vinmec Central Park International General Hospital.
Current experimental and epidemiological data indicate a strong link between the pathogenesis of Helicobacter pylori and autoimmune skin diseases. The H. pylori antigen activates T cells to cross-react and produce autoantibodies. Microbial heat shock proteins (HSPs) play an important role in the pathogenesis of autoimmune diseases because of their high degree of sequence similarity to human HSPs.
1. Pathogenesis of helicobacter pylori and autoimmune skin diseases
Autoimmune skin diseases are characterized by dysregulation of the immune system resulting in a loss of tolerance to autologous skin antigens. The long-term interaction between bacteria and host immune mechanisms makes Helicobacter pylori (H. pylori) a plausible infectious agent for autoimmunity.
Current experimental and epidemiological data indicate a strong association between H. pylori infection and the development of many extragastric diseases, including some allergic and autoimmune diseases. The H. pylori antigen activates T cells to cross-react and produce autoantibodies. Microbial heat shock proteins (HSPs) play an important role in the pathogenesis of autoimmune diseases because of their high degree of sequence similarity to human HSPs.

Stresses of physical, chemical or biological origin, as well as diseases such as cancer can cause the accumulation of heat shock proteins essential for the survival of cancer cells.
Elimination of H. pylori infection has been shown to be effective in some patients with chronic autoimmune urticaria, psoriasis, alopecia areata, and Schoenlein-Henoch purpura. There are conflicting and controversial data on the pathogenesis of helicobacter pylori with Behçet's disease, scleroderma, and autoimmune bullous diseases. There are no data to assess the association of H. pylori infection with other autoimmune skin diseases, such as vitiligo, cutaneous lupus erythematosus, and dermatomyositis.
2. The relationship between Helicobacter pylori and skin diseases
The link between infection and autoimmune problems has been gradually established over the past 25 years. Since the identification of the bacterium Helicobacter pylori (H. pylori) in 1983, more and more knowledge has been gathered, with this causative agent being directly implicated in the pathogenesis of several Venereal diseases. H. pylori is a widespread bacteria, with nearly 50% of the Western population and more than 80% of those living in developing countries infected with the bacteria. The bacteria have the amazing ability to survive in the bodies of infected people for decades and have been closely associated with humans at least since they first migrated out of East Africa about 60,000 years ago. . Current experimental and epidemiological data indicate a strong association of H. pylori infection with the development of many extragastric diseases, including some allergic and autoimmune diseases.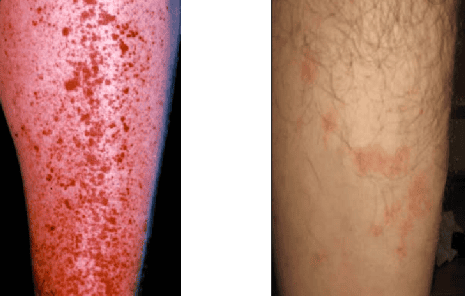
Left image: Schoenlein-Henoch purpura in a patient infected with H.Pylori.
Right image: Remission after H.Pylori eradication
3. H. pylori immune mechanisms in autoimmune disease
Various mechanisms have been proposed in an attempt to explain the extraintestinal autoimmune manifestations of H. pylori infection.
Autoimmune diseases are characterized by dysregulation of the immune system leading to an inability to tolerate autoantigens. The exact etiology of most of these diseases is unknown, but a complex process, including genetic predisposition, hormonal balance, and environmental factors such as infectious agents is thought to be play a key role. The inflammatory response to H. pylori infection can lead to the development of antigen-antibody complexes or cross-reactive antibodies leading to autoimmunity. H. pylori-induced molecular mimicry may also lead to humoral and cell-mediated autoimmune responses with the development of organ-specific as well as systemic immune pathology.
H. pylori infection induces a significant immunomodulation, often triggered by chronic inflammation, and leads to a predominant Th1 T-cell response, leading to production of interleukin (IL)-2 and interferon gamma. This chronic infection is also characterized by higher levels of local and systemic proinflammatory cytokines such as tumor necrosis factor-α, IL-6, IL-10 and IL-8. Chronic H. pylori infection can also lead to uncontrolled growth and proliferation of CD5+ B cells, which produce multiactive and self-reactive IgM and IgG3 antibodies.

Several recent reports suggest that regulatory T cells (Tregs) and dendritic cells (DCs) have tolerogenic activity in mediating the systemic immunomodulatory effects of H. pylori infection. Evidence for a functional role of Tregs and Treg-derived cytokines in promoting H. pylori-induced immunoregulation has been provided in experimental infection models. Peripheral induced induced T-regulatory cells are thought to initiate and maintain peripheral immune tolerance through energy induction, autophagy, and guidance of T-cell differentiation. inducible T regulatory cells.
These tolerant dendritic cells function by converting immature T cells to FoxP3+ Tregs through antigen presentation in the absence of co-stimulatory or cytokine signaling and appear to play a central role in the induction and maintenance of specific immunity of H. pylori. Tolerance and immunomodulation. H. pylori is also capable of potently reprogramming dendritic cells towards tolerance by efficiently inducing FoxP3 expression in immature T cells in a tumor growth factor-dependent manner ( TGF)-β.
Based on these observations it is accepted that the presence or absence of H. pylori infection may influence the risk of developing a number of autoimmune conditions, including immune-mediated dermatological diseases.
4. Conclusion
Autoimmune skin diseases are characterized by dysregulation of the immune system resulting in a loss of tolerance to autologous skin antigens. The prolonged interaction between bacteria and host immune mechanisms makes H. pylori a plausible infectious agent for autoimmunity activation. The H. pylori antigens were found to activate T cells that cross-react and produce autoantibodies. Furthermore, microbial heat shock proteins (HSPs) play an important role in the pathogenesis of autoimmune diseases because of their high degree of sequence homology with human HSPs.
Elimination of H. pylori infection has been shown to be effective in some patients with chronic autoimmune urticaria, psoriasis, alopecia areata, and Schoenlein-Henoch purpura. There are conflicting and controversial data on the association of H. pylori infection with Behçet's disease, scleroderma, and autoimmune bullous diseases. There are no data evaluating the association of H. pylori infection with other autoimmune skin diseases, such as vitiligo, cutaneous lupus erythematosus, and dermatomyositis. Epidemiological and clinical studies are needed to investigate the association between H. pylori and these diseases.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
References:
Eli Magen and Jorge-Shmuel Delgado. Helicobacter pylori and skin autoimmune diseases. World J Gastroenterol. 2014 Feb 14; 20(6): 1510–1516.














