This is an automatically translated article.
Article by Doctor Vu Duy Dung - Department of General Internal Medicine - Vinmec Times City International Hospital.The first question when a patient presents to the clinic with a first transient exacerbation is whether the seizure is likely to be epileptic, based on patient inquiries and eyewitness information.
1. Seizure factors
Risk factors for precipitating seizures, such as insomnia, and exposure to alcohol or drugs, need to be sought. In about 20% of cases, patients may have a history of absence, myoclonic, or self-aware partial seizures that were not previously known to the patient as indicative of an association. new-onset epilepsy.
A complete medical history and examination should determine whether or not the patient has evidence of an acute symptomatic seizure (eg, a persistent focal neurological deficit, persistent impairment of consciousness, or fever) requires urgent procedures including brain imaging, blood tests, and lumbar puncture to find the cause of infection. Examination should evaluate for possible injury from a convulsive seizure, such as tongue bites, lacerations, back pain from compression fractures, or shoulder pain from dislocation.
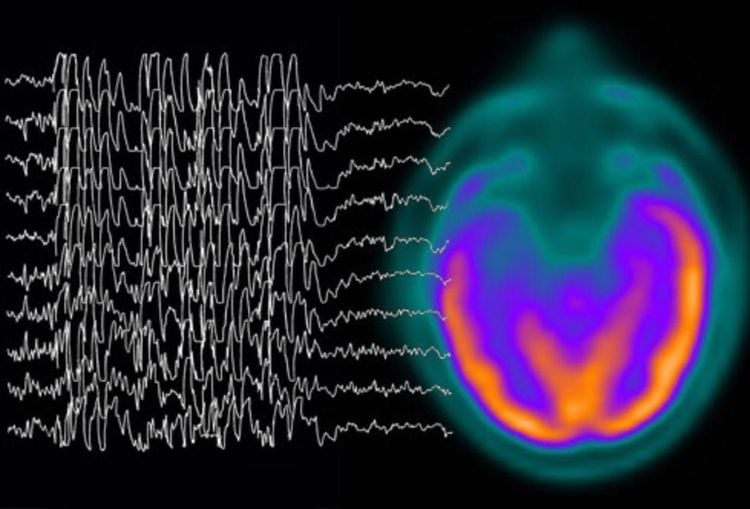
Recent advances in epilepsy definition and classification have aligned the diagnosis of epilepsy with the indication for treatment. Patients with a first seizure, a seizure-inducing structural abnormality on brain imaging and/or epileptic epileptic activity on the EEG, have a higher than 60% risk of recurrence after a second seizure. The head had no precipitating factors and was considered to have epilepsy. These patients will often benefit from antiepileptic drugs, which are also considered for patients after an initial nocturnal seizure.
2. Diagnosis of epilepsy Type of epilepsy: Partial or total
Having a specific epileptic syndrome Local: localized with onset in the frontal, temporal, or parietal region; dominant hemisphere Seizure type
Seizure description (patient and witness information; seizure classification) EEG results (out of attack, during attack)
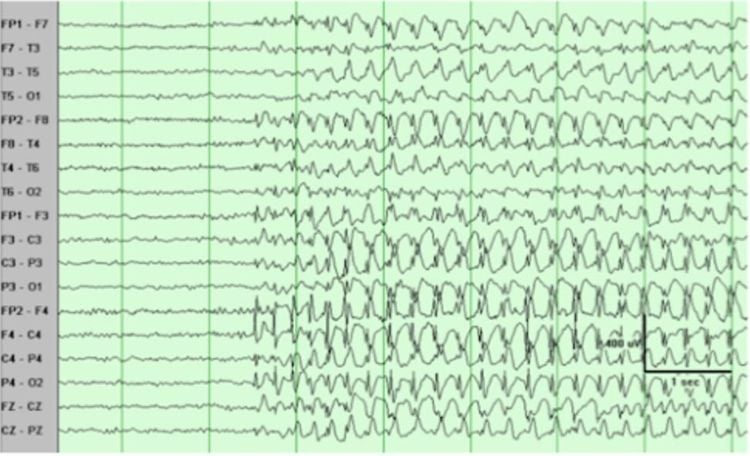
Điện não đồ (EEG) động kinh xuất hiện các hoạt động kịch phát gai nhọn sóng
Seizure pattern according to the International Federation against Epilepsy (basic, advanced classification) Seizure frequency, triggers, duration, awareness of seizures, risk factors Cause
Transition structure Genetics Immune infection Unknown Comorbidities
Non-epileptic seizures Depression, anxiety, attention deficit hyperactivity disorder Migraine Cognitive impairment Death, sudden death in epilepsy (SUDEP) Illness Patients with a precipitating seizure are generally not treated but will be counseled on lifestyle changes and, if necessary, referred to alcohol or substance abuse treatment. A or not. Acute brain injury has a risk of subsequent seizures in up to 20% of patients but is not a valid reason for prolonged seizure prophylaxis, even if the injury is accompanied by seizures or status early epilepsy. The exception is the possibility of a penetrating head injury and herpes encephalitis, since these conditions are associated with a 50% risk of developing epilepsy.

Các cơn động kinh triệu chứng cấp tính có thể điều trị tạm thời bằng cách dùng thuốc
Brain imaging
Patients with a first-time seizure require neuroimaging. Emergency imaging should be performed in any patient with a new neurological deficit, persistent change in mental status, recent trauma, or persistent headache. CT is often used as the first-line imaging modality because of its ease of access and should be considered for patients with new-onset seizures seen in the emergency room to evaluate for an acute brain injury, eg, stroke, bleeding, or trauma, and often after CT there will be a more accurate brain MRI with or without contrast injection.
Standard MRI and CT scan procedures often fail to detect lesions associated with chronic epilepsy; For this reason, an MRI should be done with a procedure that specializes in epilepsy. These lesions usually do not require urgent intervention and are expected to be better evaluated during follow-up. Using an epileptic procedure MRI, talk with the radiologist about suspected seizures before reading the results, and review the imaging results with a neuroimaging specialist who will doubles the sensitivity in detecting subtle abnormalities that can be treated with surgery.
Emergency electroencephalogram (EEG)
EEG is indicated for patients with delayed seizure recovery, fluctuating mental status, or neurologic deficits not explained by imaging findings . Routine EEG is not sufficient to detect subclinical seizure activity, which is detected only when measured within the first 30 min in 1⁄4 patients with subclinical seizures on follow-up. long and within the first 2 hours in 1⁄2 of these patients. Value goes up to over 90% with 24 to 36 hour continuous recording.
Điện não đồ (EEG) giúp các bác sĩ chẩn đoán tình trạng động kinh ở người bệnh
EEG recording after a new-onset seizure may reveal epileptic activity and help determine possible seizure patterns and risk of recurrence after the first episode. Of patients with new-onset seizures, 29% will have an epileptic pattern abnormality on the EEG. An initial EEG is particularly valuable in patients predisposed to generalized seizures. These patients have a higher frequency of seizure-like discharges than with partial seizures and a characteristic response to activation tests of hyperventilation and light stimulation. The EEG in generalized epilepsy can be normal with appropriate treatment, and it is important to record the EEG before treatment. There is a slight increase in the likelihood of capturing epileptic abnormalities on the EEG in patients 24 to 48 hours after a new-onset seizure. However, acute changes in the EEG may reflect the consequences of acute brain injury or the consequences of a seizure and may not necessarily predict the risk of future seizure recurrence. Patients presenting with an epileptic seizure require at least one EEG and one brain imaging because it is not uncommon to find a small structural abnormality or an EEG indicating a predisposition to seizures. total seizure.
Source:
Stephan US. Evaluation of Seizure Etiology From Routine Testing to Genetic Evaluation. Continuum (Minneap Minn) 2019;25(2, Epilepsy):322–342
Please follow the series of articles on "Evaluating seizure causes from routine tests to genetic testing" by Dr. Vu Duy Dung including:
Part 1: Evaluation of epilepsy causes from tests routine referral to genetic testing Part 2: New-onset seizures Part 3: Epileptic assessment Part 4: Extra-genetic causes of epilepsy Part 5: Genetic causes of epilepsy