This is an automatically translated article.
Article by Doctor Vu Duy Dung - Department of General Internal Medicine - Vinmec Times City International General HospitalCauses of epilepsy can be divided into six different groups: structural, metabolic, genetic, infectious, immunological and unknown. The etiologies are not mutually exclusive, allowing a structural-genomic cause in patients with tuberous sclerosis or a metabolic-gene cause in patients with epilepsy associated with congenital metabolic disorders.
The generalized epilepsy includes four epileptic syndromes that are still considered idiopathic generalized seizures: childhood absence seizures, juvenile absence seizures, juvenile myoclonic epilepsy, and other myoclonic epilepsy. isolated generalized tonic-clonic seizures. Generalized genomic epilepsy also includes the group of patients with epileptic encephalopathies, often with a specific genetic cause.
1.Structural Most patients with epilepsy need high-resolution epilepsy-specific procedural brain MRI to assess the possibility of a structural cause. Exceptions may be in patients with a convincing history and classic EEG findings of idiopathic generalized epilepsy. The presence of an epileptic and resectable lesion should trigger an evaluation for surgery in patients with drug-resistant epilepsy. In patients with refractory focal epilepsy and a normal MRI, fludeoxyglucose positron emission tomography (FDG-PET) is useful in finding an area of decreased metabolism.
2. Metabolism Congenital metabolic-associated seizures often have features of an epileptic encephalopathy with episodes that begin at a young age, are often refractory to antiepileptic drugs, and are associated with severe cognitive, sensory and/or motor impairment. Most metabolic epilepsy is thought to have an underlying genetic abnormality. They are specifically grouped according to the biochemical pathway involved and age of onset. The presence of other neurologic abnormalities, such as movement disorders and ataxia, systemic symptoms, parental pedigree, and a positive family history of a similar disease, may are suggestions. General examination should look for dysmorphic features and an abnormal head circumference. Skin and hair abnormalities may predispose Menkes syndrome or biotinidase deficiency. Eye examination is necessary in identifying signs of retinitis pigmentosa (neuronal ceroid lipofuscinosis, mitochondrial diseases), cherry red spots in blind spots (gangliosidosis, Niemann-Pick disease), vitreous displacement cataracts (sulfite oxidase deficiency), and cataracts (serine biosynthesis defect). A select number of inborn metabolic errors may manifest in adolescents and adults and requires systematic evaluation for biochemical abnormalities and genomic etiology.

Các bất thường về da và tóc của hội chứng Menkes
3. Infection Infections cause not only acute symptomatic seizures in the early stages of infection, but can also lead to late seizures far from the onset of the infection and its treatment. Consistent with the treatment of epilepsy. Infectious causes include brain flukes, viral encephalitis, bacterial meningitis, fungi, tuberculosis, toxoplasma, malaria, and HIV.
Brain flukes are more common in developing countries and are often the leading cause of epilepsy in those countries. Seizures can occur at any stage of cyst formation. Seizures during the acute phase of bacterial meningitis are a poor prognostic sign and are associated with increased mortality. Late epilepsy occurs in about 5% to 10% of patients who survive bacterial meningitis. Epilepsy associated with viral encephalitis is most commonly associated with herpes simplex type 1, in 50% of patients. Acute seizures are a symptom of herpes simplex type 1 infection with a similar incidence. Cytomegalovirus is the most common fetal viral infection and can cause multiple cortical developmental anomalies and cortical calcifications, with seizures usually manifesting during the first month of life. Subacute sclerotic encephalitis is a chronic, progressive disease associated with first measles infection before 2 years of age.
Acute symptomatic seizures are seen in influenza B, varicella, measles, mumps, rubella, and West Nile virus, but information is limited on the possibility that acute viral encephalitis often leads to delayed seizures or not. About 50% of congenital Zika virus infections are accompanied by seizures, which are characteristic in the first months of life. Tuberculous vasculitis and cortical tuberculous neoplasms can lead to seizures. Seizures in cerebral toxoplasmosis are typically associated with reactivation of a latent infection in immunocompromised individuals.
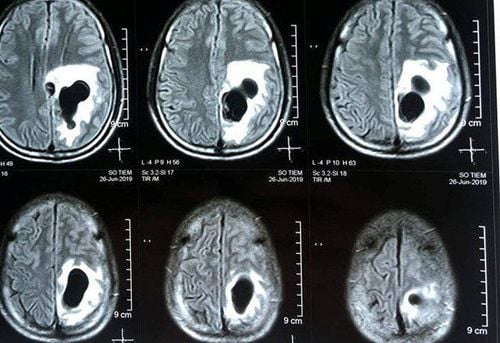
Hình ảnh sán làm tổ trong não của người bệnh trên hình ảnh chụp cộng hưởng từ
4. Inflammation Increasingly, autoimmune antibody syndromes are recognized as a cause of epilepsy. Most of these antibodies are directed against antigens on neuronal surfaces, including synaptic neurotransmitter receptors, ion channels, or related proteins. A second group has antibodies specific to nuclear antigens in the neuron or cytoplasm. Both groups had an association with cancer risk, as high as 90% in patients with nuclear or cytoplasmic antibodies. Thyroid antibodies are seen in patients with steroid-responsive encephalopathy and in patients with high levels of glutamic acid decarboxylase 65 antibodies may present with immune-mediated epilepsy.
Patients with autoimmune epilepsy often present a high frequency of refractory seizures and/or status epilepticus. In addition to the high frequency of seizures and treatment resistance, patients often have progressive mental status changes, neuropsychiatric symptoms, autonomic dysfunction, viral signaling, and sometimes regional dyskinesia. face or face-arm. Tests may reveal CSF consistent with inflammation, medial temporal lobe hyperintensity on T2 pulses, and accompanying cancer on screening. In patients with longer-lasting epilepsy who may not initially present as an emergency, the value of a positive antibody test can be predicted by the Circulating Antibody in Epilepsy (APE) score on the 4, has a sensitivity of 82.6% and a specificity of 82.0%. This scale has been demonstrated in a large cohort of epilepsy patients and has a sensitivity of 97.7% in patients with unexplained epilepsy for predicting the presence of an autoimmune antibody, seen in 43 out of 87 patients.

Xét nghiệm dịch não tuỷ giúp đánh giá tình trạng viêm nhiễm
Source:
Stephan US. Evaluation of Seizure Etiology From Routine Testing to Genetic Evaluation. Continuum (Minneap Minn) 2019;25(2, Epilepsy):322–342
Please follow the series of articles on "Evaluating seizure causes from routine tests to genetic testing" by Dr. Vu Duy Dung including:
Part 1: Evaluation of epilepsy causes from tests routine referral to genetic testing Part 2: New-onset seizures Part 3: Epileptic assessment Part 4: Extra-genetic causes of epilepsy Part 5: Genetic causes of epilepsy