This is an automatically translated article.
The article is professionally consulted by Master, Doctor Vu Van Quan - Gastroenterologist - Department of General Surgery & Anesthesiology - Vinmec Hai Phong International General HospitalUnlike a pancreatic cyst, a pancreatic pseudocyst is a reactive cyst that forms to localize pancreatic juice when it has leaked from the pancreatic parenchyma. Because it is only surrounded by a very thin cyst wall, a large amount of pancreatic enzymes can be released into the peritoneum at any time, causing serious consequences. The information on pancreatic pseudocysts is intended to help control and monitor patients, search and intervene if there are pancreatic pseudocysts after acute pancreatitis.
1. What is a pancreatic pseudocyst?
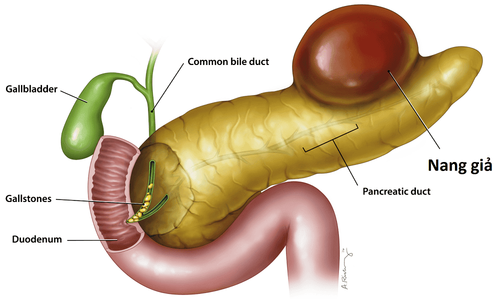
The pancreas is an organ located behind the stomach that secretes digestive enzymes through the pancreatic duct into the small intestine. The pancreas also belongs to the endocrine system when it produces the hormone insulin, which is secreted directly into the circulation to help control blood sugar levels.
Acute pancreatitis occurs when there are activated inflammatory reactions in the pancreatic parenchyma. When the pancreas becomes inflamed, it can leak digestive enzymes. This further damages the pancreatic parenchyma. To overcome this situation, the intra-abdominal fascia reaction will form fibrous tissue, aiming to localize pancreatic juice. It is this mechanism that causes the formation of pancreatic pseudocysts.
Thus, a pancreatic pseudocyst is an aneurysm containing a small amount of pancreatic fluid leaking out of the pancreas. They can form right next to the pancreas during acute pancreatitis processes.
Pancreatic pseudocyst is completely different from true pancreatic cyst. While both pancreatic cysts and pancreatic pseudocysts are aggregates of pancreatic fluid, a true pancreatic cyst is a self-contained structure, with a cell layer separating it from nearby tissue; In contrast, a pancreatic pseudocyst is a closed sac and does not have a layer of epithelial cells separating it from nearby tissues. This distinction is very important to help guide the intervention.
In addition, some pancreatic cysts can be a pancreatic cancerous mass while pancreatic pseudocysts are rarely cancerous. However, if they are large, they may need to be drained, avoiding the risk of causing pain or rupture, spreading pancreatic juice causing chemical peritonitis or pancreatic pseudocyst is also a favorable environment for pancreatic cancer. infection.

2. What causes pancreatic pseudocyst?
Unlike pancreatic cysts, which form spontaneously, pseudocysts form when the cells of the pancreas become inflamed or damaged, and pancreatic enzymes begin to leak out. It is the leakage of pancreatic enzymes that harms not only the healthy tissues of the pancreas but also the surrounding organs.Pancreatic pseudocysts can develop after a sudden episode of acute pancreatitis. However, people with chronic pancreatitis can also develop pancreatic pseudocysts because they can form in the setting of episodes of acute pancreatitis against a background of chronic pancreatitis.
Presence of gallstones causing obstruction of the pancreatic duct and excessive alcohol consumption are the two most common causes of pancreatitis and thereby the formation of pancreatic pseudocysts. In addition, there are some other causes as follows:
Injury to the pancreas Pancreatic infection Pancreatic tumor High blood calcium levels Very high blood triglyceride levels Drug damage to the pancreas Autoimmune disease Cystic fibrosis hereditary

3. What are the symptoms of pancreatic pseudocyst?
Symptoms of pancreatitis and pancreatic pseudocyst formation are as follows:
Abdominal pain, pain spreading around the back Fever Stomach bloating Nausea and vomiting If pancreatitis is severe, pseudocyst formation can also cause dehydration, low blood pressure. Sometimes the patient's condition becomes critical quickly, organ dysfunction and circulatory collapse. At the same time, if the pancreatic pseudocyst ruptures, it also causes similar complications.
However, the formation of pancreatic pseudocysts is sometimes without any symptoms. The presence of this cystic mass was discovered incidentally during intra-abdominal imaging for another pathology.
4. How is pancreatic pseudocyst diagnosed?
The diagnosis of pancreatic pseudocyst will be based on the history, clinical symptoms and laboratory tests, including:
Quantitative tests of pancreatic enzyme levels in the blood and also in the urine. Tests to assess the status of the body's internal metabolism such as complete blood count, measurement of electrolytes sodium, potassium, calcium, glucose, blood triglycerides... Imaging tests, which may include ultrasound abdomen or abdominal computed tomography (CT scan). If the evidence to distinguish pancreatic cysts from pancreatic pseudocysts is still unclear, the patient may need to have magnetic resonance imaging (MRI) or ultrasound instruments, especially endoscopic ultrasound. In cases where the diagnosis is still undecided, the doctor will need to take a sample of the fluid in the cyst for testing. The instrument used is a long, thin needle inserted into the tumor under radiological guidance. Results will help distinguish pancreatic cyst, pancreatic pseudocyst, abscess or pancreatic cancer.

5. How are pancreatic pseudocysts treated?
Treatment of pancreatic pseudocyst usually consists of two parts: (1) treatment of pancreatitis and (2) treatment of pseudocyst. To treat pancreatitis, the patient is given the following:
Bed rest, limited exercise Intravenous electrolyte solutions Pain relievers Antiemetics so that the pancreas can rest or nourish through the nose through the nasogastric tube to the small intestine without going through the duodenum - ie without the involvement of the pancreas. Treatment for pseudocysts and pancreatic pseudocysts can vary. Many cases of small pancreatic pseudocysts will shrink and disappear on their own while treating acute pancreatitis alone. However, the patient still needs periodic re-examination with imaging to rule out the possibility of the pancreatic pseudocyst forming again. In case the pancreatic pseudocyst is large, the patient needs to be drained the pancreatic juice in the cyst out through the skin or surgically removed the pancreatic pseudocyst.

6. Possible complications of pancreatic pseudocyst
Pancreatic pseudocysts are sometimes harmless, but they can also cause serious problems. They can even be fatal if not treated immediately. Fortunately, most of these cases are quite rare.Possible complications from pancreatic pseudocysts include:
Infection, which can lead to sepsis and septic shock. Intracystic hemorrhage Hemorrhage into the spleen Thrombotic formation in the splenic vein Obstruction of the common bile duct by the cyst, causing jaundice, yellowing of the eyes, portal hypertension, Obstruction of gastric outlet, Pancreatic cyst rupture When pancreatic pseudocyst causes If one of the above complications occurs, emergency surgery or interventional drainage in the cyst is always indicated.
To summarize, a pancreatic pseudocyst is a sac that contains pancreatic fluid when it has leaked out. This condition may have no symptoms but can sometimes cause serious problems, sometimes even more than acute pancreatitis, if there is a massive release of pancreatic enzymes into the peritoneum. Therefore, early detection of the presence of pancreatic pseudocysts after acute pancreatitis events and proactive intervention is essential to help prevent serious complications later.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.