This is an automatically translated article.
Posted by Master, Doctor Pham Thi Mai Thanh - Department of General Internal Medicine - Vinmec Times City International HospitalPancreatic pseudocyst and septal necrosis is a condition that needs to be detected, diagnosed correctly and treated promptly to prevent life-threatening danger to the patient.
1. Definition of pancreatic pseudocyst and walled necrotic foci
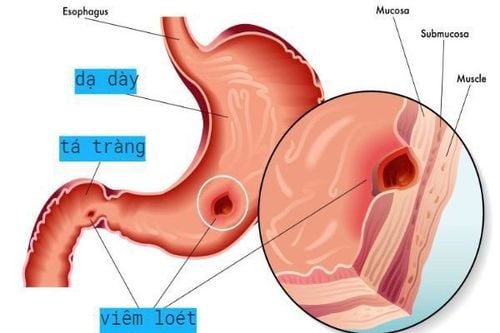
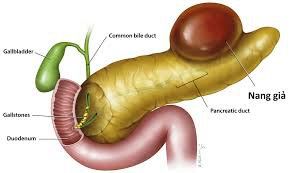
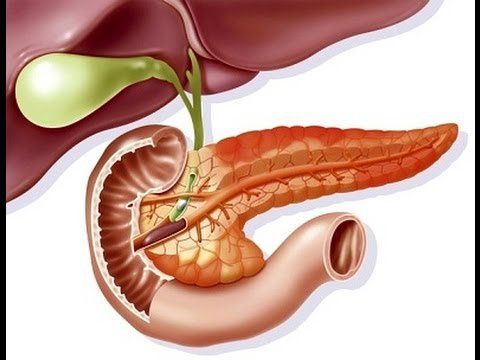
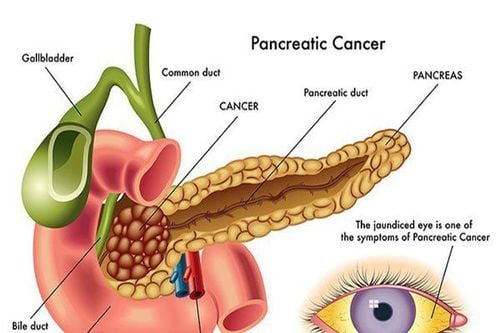
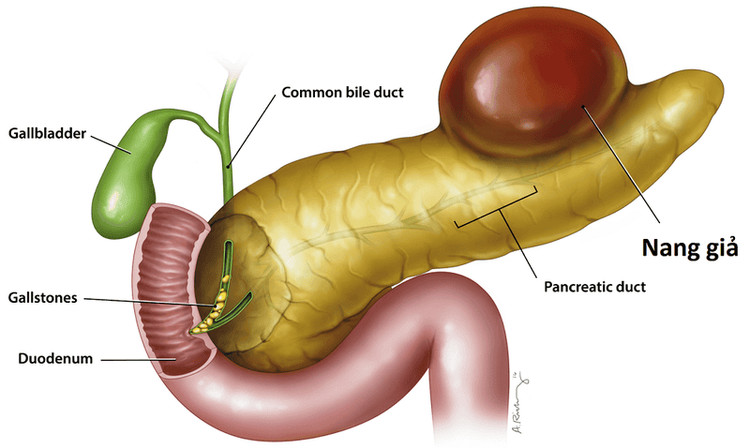
Pancreatic pseudocyst and wall of pancreatic necrosis (WOPN) are often complications of acute pancreatitis but can also be seen in patients after pancreatic trauma, defined as follows:Pancreatic pseudocyst : Chronic fluid accumulation Outside of the pancreas has a clear shell, with little or no necrosis, with a septal fovea: A chronic fovea of pancreatic or parapancreatic necrosis that develops from an inflammatory site, has a clear wall, and persists for at least 4 weeks stage of acute pancreatitis. Necrotic foci may contain fluid and solid components concentrated in clusters or not, in the pancreas or outside the pancreas. Diagnosis: The diagnosis of pancreatic pseudocyst or septal necrosis is seen in the presence of an encapsulated fluid collection in a patient with a history of pancreatitis or pancreatic trauma. If the diagnosis is uncertain because the clinical picture is unclear or the ultrasound or CT images are atypical, endoscopic ultrasonography can be performed to obtain samples from the fluid or cyst wall for testing.
Early pharmacological CT can rule out pseudoaneurysms in patients considering cyst drainage.
For the differential diagnosis of septal necrotic foci from pancreatic pseudocyst alone, MRI is preferable to CT.
Comparison of images with previous radiographs is necessary, if the cyst is present before acute pancreatitis or trauma, it is usually a pancreatic cyst, not a pseudocyst.
2. Treatment of pancreatic pseudocysts and necrotic foci with septa
Follow-up: Clinical and imaging follow-up for patients with no or very few symptoms. Monitor pancreatic pseudocysts with contrast-enhanced CT or MRI every 3-6 months. No further follow-up is required for cysts that resolve or decrease in size and are asymptomatic. CT or MRI should be done 3 months earlier if the patient presents with abdominal pain, jaundice, rapid appetite, or fever.Supportive treatment: All patients with pancreatic pseudocyst or septal necrosis need nutritional assessment and supportive treatment with intravenous nutrition or medication if necessary
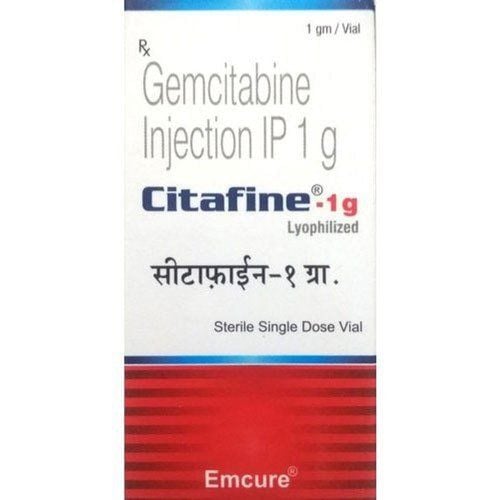
Nose-enteral feeding: Do reduce the need for endoscopic intervention because of pain relief and improved nutritional status. PPIs: Reduce gastric acid secretion and decrease pancreatic bicarbonate secretory response Somatostatin receptor agonist: Octreotide 50-200mcg subcutaneously every 8 hours reduces pancreatic secretion, indicated for patients with pancreatic fistula Patients have clinical symptoms such as pain, fever, jaundice ... cysts increase in size rapidly or are infected but drug treatment does not help with indications for cyst drainage.

Transmural drainage: Transluminal stenting of the stomach/duodenum and cyst wall Transpapillary drainage: Placement of a trans-cystic stent that connects to the pancreatic duct Efficacy: Endoscopic pseudocyst drainage can success rate is 90%, cure rate is 70-80%, recurrence rate is 10-15%. The success rate will be lower with a walled necrosis because there is a higher rate of infection and the solid component is more difficult to drain. The recurrence rate can increase up to 30%.
Complications of endoscopic drainage can be: Secondary infection, bleeding, perforation, stent fall into the cyst.
Percutaneous cyst drainage: Used to decompress the peripancreatic fluid collection and stabilize the patient's blood infection before surgery if endoscopic intervention is not possible.
Surgery: In both cases of infectious or non-infectious foci of pancreatic necrosis but with symptoms such as low-grade fever, nausea, lethargy and anorexia, pancreatectomy is indicated. The purpose of this surgery is to remove the necrotic part of the pancreas, preserve the functioning pancreas, control the pancreatic fistula, and limit damage to nearby organs.
Vinmec International General Hospital with a system of modern facilities, medical equipment and a team of experts and doctors with many years of experience in medical examination and treatment, patients can rest assured to visit examination and treatment at the Hospital.
SEE MORE
Pancreatic pseudocyst: What you need to know How dangerous is acute pancreatitis? How does chronic pancreatitis happen?
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.