This is an automatically translated article.
The article is professionally consulted by Master, Doctor Phan Ngoc Toan - Emergency Medicine Doctor - Emergency Department - Vinmec Danang International Hospital.It is very common for patients to experience severe pain in the ICU, and understanding the location and nature of the pain plays a very important role in deciding on an emergency regimen. The use of sedative analgesics in emergency resuscitation is also a major part of treatment.
1. What is a sedative pain reliever?
Patients in the critical ward or the intensive care unit are often awake, so they are very worried due to being isolated, hearing many alarms of medical machines and suffering a lot of pain, especially during the procedure. The use of sedative analgesics in emergency resuscitation is also part of the treatment.Depending on the pathology, the patient may have the following manifestations:
Irritability. Intravenous needle drop. Pain and instability. Anti ventilator. Fast heart. Stress. Hypertension. Or when emergency procedures are required: endotracheal intubation, lumbar puncture, endoscopic endoscopic bone marrow puncture, bronchoscopy, pleural drainage, pericardiocentesis, central venous catheterization, chiropractic...
Goals of sedation:
Patient comfort, no anxiety. Reduce stress. Allows for easy tricks. Avoid resisting the ventilator, extubate the endotracheal tube by yourself. Reduced oxygen demand. Ideal sedation relieves pain when:
Fast acting and quick to wake up. Has the desired effect time. Easy dose adjustment. Few respiratory and cardiovascular side effects, no effect on liver and kidney function. Does not interact with other drugs. The therapeutic concentration gap is large.
Thuốc giảm đau an thần giúp tăng tiết hormone dopamin
2. Some types of sedative analgesics in emergency resuscitation
2.1 Opioid pain relievers group
FentanylAdvantages: immediate onset of action and less hypotension than opioids. Cons: Stiffness of the chest wall may occur with higher doses. Role: A good choice for pain relief for most critically ill patients. Hydromorphone
Advantages: Uses lower IV doses than other opioids. Cons: Potentially neurotoxic (irritant) metabolite, which may accumulate in patients with hepatic and/or renal dysfunction. Role: Alternative analgesic option to fentanyl or morphine. Dose adjustments and titrations are necessary for patients with renal and/or hepatic impairment. Morphine sulfate
Advantages: Non-CYP metabolism (glucuronidation) Cons: May accumulate in hepatic or renal dysfunction and prolong action. Histamine release causes vasodilation, hypotension and bradycardia Role: Analgesia as an alternative to fentanyl or hydromorphone with reduced preload and myocardial depression. Dose adjustments and titrations are necessary for patients with renal and/or hepatic impairment. Avoid in patients with advanced or decompensated liver disease with renal impairment due to the risk of neurometabolite accumulation. Continuous infusions are not typically used for sedation or pain relief in the ICU but are commonly used for palliative purposes. Remifentanil
Pros: Extremely short acting. Cleared by nonspecific plasma esters to inactive metabolites. Does not accumulate in renal or hepatic failure. Promptly reverse analgesia and sedation upon discontinuation. Cons: Pain and discomfort are predictable when stopped abruptly. Excipients glycine may accumulate in renal failure. Role: An alternative to fentanyl for patients requiring frequent neurological evaluation or those with multiple organ failure.
2.2 Non-Opioid analgesics
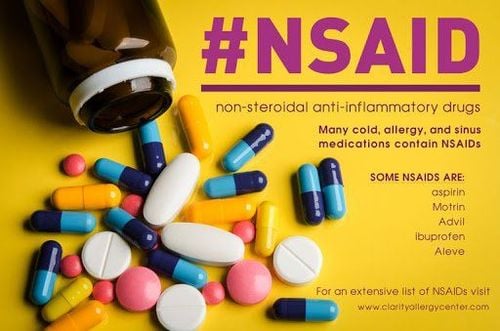
Acetaminophen (paracetamol)Advantages: Not as dependent and tolerated as opioids. There are no antiplatelet effects and gastrointestinal toxicity of NSAIDs. Cons: Lacks significant anti-inflammatory effect. IV infusion requires more than 15 minutes. May cause hepatotoxicity in chronic or acute overdose. Avoid or use lower daily doses in the elderly and in patients at risk for hepatotoxicity (eg, heavy alcohol use or malnutrition). Interactions with warfarin (possibly prolonging INR) and inducers of CYP450 (increased risk of hepatitis). Role: First choice for the treatment of mild and moderate acute pain. Adjuvant analgesics may reduce the need for opioids. When liver dysfunction is significant, consider avoiding or reducing the dose of Ketorolac
Advantages: Not as dependent and tolerable as opioids. Effective anti-inflammatory. Cons: May cause or worsen kidney failure. Dose-related risk of gastroparesis. Reversible inhibition of platelet function. May alter the cardioprotective effects of aspirin. Role: Adjuvant analgesics may reduce opioid requirements. Avoid in renal failure, gastrointestinal bleeding, platelet dysfunction, ischemic heart disease, heart failure, decreased cardiac output, hypokalemia, asthma or cirrhosis. Contraindicated in the treatment of surgical pain during coronary artery bypass graft surgery. The patient needs to make sure there is enough fluid. Ibuprofen
Advantages: No dependence and tolerance like opioids. Effective anti-inflammatory. Cons: May cause or worsen kidney failure. Dose-related risk of gastroparesis. Reversible inhibition of platelet function. May alter the cardioprotective effects of aspirin. Role: Short-term treatment of moderate acute pain and fever. Adjuvant analgesics may reduce the need for opioids. Avoid in renal failure, gastrointestinal bleeding, platelet dysfunction, ischemic heart disease, heart failure, decreased cardiac output, hypokalemia, asthma or cirrhosis. Contraindicated in the treatment of surgical pain during coronary artery bypass graft surgery. The patient needs to make sure there is enough fluid.
Gabapentin
Advantages: Effective in the treatment of neuropathic pain. Low risk of drug interactions. Cons: Oral only, scheduled dosing and individual titration over days to weeks. Oral bioavailability is variable (27 to 60%) and is inversely proportional to dose. Adverse effects include sedation, dizziness and ataxia, which may worsen in renal failure, requiring dose adjustment. It should not be stopped suddenly, due to the risk of symptom disruption. Role: Useful adjunct to other analgesics for the treatment of neuropathic pain and postoperative pain or dysfunction in patients who can be treated orally. Pregabalin
Advantages: Effective in the treatment of neuropathic pain. Oral bioavailability (>90%) is more reliable than gabapentin and may provide faster pain relief with shorter time to titrate to full dose Cons: Oral only, scheduled dosing and titration individuals for days to weeks. Oral bioavailability is variable (27 to 60%) and is inversely proportional to dose. Adverse effects include sedation, dizziness, blurred vision, dry mouth and ataxia, which may worsen in renal failure, requiring dose adjustment. It should not be stopped suddenly, due to the risk of symptom disruption. Role: Useful adjunct to other analgesics for the treatment of neuropathic pain and postoperative pain or dysfunction in patients who can be treated orally.

Thuốc giảm đau Paracetamol
2.3 Group of sedatives – muscle relaxants
PropofolAdvantages : Sedative – induces sleep with immediate onset and rapid awakening upon discontinuation of short-term use. Metabolism is unchanged in hepatic or renal impairment and has few significant drug interactions. The intravenous route is easily titrated to the desired depth of sedation, minimizing the risk of overdose. Propofol effectively reduces intracranial pressure, reduces cerebral metabolism, controls seizures, and may reduce tremors during the rewarming phase of hypothermia in cardiac arrest resuscitation. Cons: Side effects include hypotension, bradycardia, respiratory depression, decreased myocardial contractility, increased triglycerides, pain at the peripheral injection site. Specific product presentation may include potential allergens (eggs, soy, peanuts, others). No analgesic effect. Role: A good choice in combination with appropriate analgesia for short-term sedation in patients requiring rapid awakening. Also a good option for reducing intracranial pressure or for short sedation is readily available for early weaning trials. Ketamine
Advantages: Strong polar sedation with marked analgesia that helps to maintain cardiac output and mean arterial pressure without inhibiting the respiratory tract. Does not inhibit the protective reflex. May reduce acute opioid tolerance. Cons: Sympathetic stimulation (increased heart rate and myocardial oxygen demand, increased intracranial pressure and systemic blood pressure) may be intolerable depending on clinical treatment. Rarely, respiratory depression has been associated with rapid administration or higher doses. Adverse effects may include hallucinations, delirium on discontinuation, unpleasant recall, hypersensitivity, nausea and vomiting. Complex metabolism, may accumulate in renal and/or hepatic impairment or due to drug interactions. Role: An alternative option for the treatment of postoperative pain, severe agitation or as an adjuvant analgesia in patients with refractory severe pain in clinical settings with increased myocardial oxygen demand. and sympathetic tone.
2.4 Central alpha2-adrenergic agonists
DexmedetomidineAdvantages: Effective sympathomimetic sedation (central alpha2 agonist) with moderate anxiolytic and analgesia, but no clinically significant effect on respiration. The nature and degree of sedation may allow a critically ill, mechanically ventilated patient to be interactive or easily awakened, yet comfortable. May be used in non-ventilated ICU patients and continued as needed after extubation. Reduce tremors during the rewarming phase of hypothermia in cardiac arrest resuscitation. May cause less delirium than other sedating options. Cons: There is a potential for hypotension and bradycardia or hypertension that does not resolve rapidly with abrupt discontinuation of the drug. Dosage should be reduced with renal and/or hepatic impairment. Rapid administration of a loading dose may be associated with cardiovascular instability, tachycardia, bradycardia, or heart block. Does not induce the deep sedation required for neuromuscular blockade. Role: A good alternative for short- and long-term sedation in critically ill patients without associated cardiovascular conditions. May be useful for sedation of patients at high risk of developing delirium.
2.5 Benzodiazepines
Midazolam:Advantages: A potent sedative and anxiolytic agent with immediate action and short duration of action when administered short-term (<48 hours). Cons: Metabolized by the liver by CYP3A4 to active metabolites that can accumulate and cause prolonged sedation if used long-term. The half-life may be prolonged in critically ill patients with hepatic or renal impairment. Danger of delirium. In addition, it interacts with drugs used in the ICU (eg, some antiretrovirals, azole antifungals) that alter CYP metabolism such that excessive sedation may occur when administered. midazolam and drugs metabolised by CYP3A4. Role: A good option for short-term surgery and acute agitation. Dosage adjustment and gradual titration is necessary for patients with renal and/or hepatic impairment. Lorazepam
Advantages : Sedative, sedating, strong anxiolytic with anticonvulsant properties. Metabolized in the liver by glucuronidation to inactive metabolites. The risk of drug interactions is relatively low and safe in mild to moderate renal and hepatic impairment. Cons: Relatively slow onset. Risk of excessive sedation during titration due to slow response and accumulation in peripheral tissues. Danger of delirium. Risk of precipitation. The solvent propylene glycol can accumulate with prolonged use or high doses causing metabolic acidosis and organ dysfunction. The half-life is long, with a significant cumulative risk in the elderly or in patients with significant renal or hepatic impairment. Role: A good choice for sedation for most patients, including those who may require long-term continuous sedation. Although intermittent bolus doses may be preferred, continuous infusions may be initiated for patients who require higher frequently repeated dosing. Diazepam
Advantages: Quick onset with strong sedative and muscle relaxant effects.
Cons: Metabolized by the liver to active metabolites that can accumulate and cause prolonged sedation if used long term. The half-life may be prolonged in critically ill patients with hepatic and/or renal impairment. Danger of delirium. In addition, it interacts with drugs used in the ICU that alter CYP metabolism. The injection solution contains propylene glycol solvent and cannot be given as a continuous infusion. Injection site pain and risk of phlebitis.
Role: Rarely used for sedation of critically ill patients. May be useful for seriously ill patients at risk of alcohol withdrawal or seizures from drug overdose or poisoning.

Sử dụng các loại thuốc giảm đau an thần trong hồi sức cấp cứu cũng là một phần trong điều trị
To register for examination and treatment at Vinmec International General Hospital, you can contact Vinmec Health System nationwide, or register online HERE.
MORE:
What to know about Seretide Asthma Spray Antiarrhythmic Cordarone Medication Notes when using nasal drops containing Xylometazoline