This is an automatically translated article.
Posted by Master, Doctor Pham Thi Thu Huong - Head of Department of Gastroenterology - Endoscopy - Department of Gastroenterology - Endoscopy - Vinmec Times City International HospitalPeople with GERD experience uncomfortable symptoms or damage to the esophagus as a result of acid reflux. Symptoms of GERD can include heartburn, regurgitation, and difficulty swallowing or pain when swallowing.
People with gastroesophageal reflux disease (GERD), also known as "acid reflux" occurs when gastric juices back up into the esophagus and/or mouth. Occasional reflux is normal and can occur in otherwise healthy infants, children, and adults, most often after eating a meal. Most reflux episodes are brief and do not cause uncomfortable symptoms or complications. In contrast, people with GERD experience uncomfortable symptoms or damage to the esophagus as a result of acid reflux. Symptoms of GERD can include heartburn, regurgitation, and difficulty swallowing or pain when swallowing.
1. What happens in acid and gerd reflux?
When you eat, food is carried from your mouth to your stomach through your esophagus - a tube structure about 25cm long and 2.5cm wide in adults. The esophagus is made up of layers of tissue and muscle that can stretch to push food into your stomach through a series of wave-like movements called peristalsis.At the lower end of the esophagus, where it connects to the stomach, there is a circular muscle called the lower esophageal sphincter. After you swallow, the Stomach expands to allow food to enter your stomach, which is then mixed with stomach acids for the food to be digested. The Stomach then contracts to prevent food and acid from flowing from your stomach into your esophagus.
However, sometimes CSOs are not elastic; This allows stomach contents to back up into the esophagus. Most reflux episodes occur shortly after a meal, are brief, and cause no symptoms. Normally, reflux rarely occurs during sleep.
In some people, acid reflux causes uncomfortable symptoms or damage to the esophagus over time; When this happens, it's called GERD. In general, damage to the esophagus is more likely to occur when acid reflux is frequent, the stomach increases acid secretion, or the esophagus cannot remove acid quickly.
2. GERD Risk Factors

Những người béo phì hoặc thừa cân tăng nguy cơ mắc bệnh GERD
Diaphragmatic hernia: This is a condition in which part of the upper stomach pushes up through the diaphragm (the large, flat muscle at the base of the lungs). The diaphragm has an opening for the esophagus to pass through before it joins the stomach; in people with a hernia, part of the stomach is also contracted through this hole. Obesity: People who are obese or overweight have an increased risk of GERD. While the cause is not fully understood, this is thought to be related to an increase in intra-abdominal pressure. Pregnancy: Many women experience acid reflux during pregnancy. This condition usually resolves after birth, and complications are rare. Lifestyle factors and medications: Certain foods (including fatty foods, chocolate, and mints), caffeine, alcohol, and tobacco can all cause acid reflux and GERD. Some medications also increase this risk.
3. GERD warning symptoms
The most common symptoms of GERD are:Heartburn: This is usually a burning sensation in the epigastrium, sometimes spreading to the throat. It usually happens after a meal. Regurgitation: This is when stomach contents (acids mixed with undigested food) back up into your mouth or throat. Other symptoms of GERD may include:
Stomach pain (upper abdominal pain) Chest pain Difficulty swallowing or pain when swallowing Persistent laryngitis/hoarseness (caused by acid irritating the vocal cords) Sore throat or persistent cough Persistent feeling of choking in the throat Nausea and/or vomiting Over time, GERD can lead to complications. These include problems related to damage to the esophagus as well as other problems. The following signs and symptoms may indicate a more serious problem. Tell your doctor right away if you have the following symptoms:
Difficulty swallowing or pain when swallowing (e.g., feeling like food is stuck in your throat) Feeling like you are choking Loss of appetite or loss of appetite weight without trying Chest pain Signs of gastrointestinal bleeding, such as blood in vomit or dark-colored vomit that looks like coffee grounds or black stools Persistent vomiting New stomach pain and 50 years old and up

Ợ nóng, ợ trớ là dấu hiệu phổ biến nhất của GERD
4. Diagnosis of GERD
Diagnosing GERD is based on your symptoms as well as other risk factors.Diagnosis based on symptoms: Doctors can diagnose GERD based solely on "classic" GERD symptoms (heartburn and/or regurgitation). In this situation, they may recommend a trial of medication; If your symptoms improve, it's likely GERD is the cause.
Additional testing: Your doctor may recommend additional evaluation and testing if you:
● No improvement in symptoms after taking a proton pump inhibitor
● No classic symptoms of GERD ( heartburn or reflux)
Have symptoms that suggest a more serious problem
Have risk factors for certain complications such as Barrett's esophagus
It is important to rule out problems Potentially life-threatening problems can cause symptoms similar to those of GERD. For example, chest pain can also be a symptom of heart disease and should be evaluated immediately.
If life-threatening problems have been ruled out and the diagnosis of GERD is unclear, your doctor will likely recommend one or more of the following tests.
Upper Gastrointestinal Endoscopy: Endoscopy allows the doctor to examine the upper digestive tract directly. A small, flexible tube is inserted into the esophagus, stomach, and small intestine, with a light source and a camera that displays magnified images on a screen, to help assess gastrointestinal damage and take a small tissue sample (biopsy). ) to determine the extent of tissue damage. 24-hour esophageal pH measurement: This is the most direct way to measure acid reflux frequency. Testing involves inserting a thin tube with a sensor through the nose and into the esophagus (which is left in place for 24 hours); Another method is to place a wireless sensor into your esophagus during an upper endoscopy. For 24 hours, you will be asked to keep a diary of your symptoms. The sensor measures how often stomach acid backs up into your esophagus. Your doctor can use this information to determine the frequency of your reflux and how it relates to your symptoms. This test can be used to confirm the diagnosis of GERD if you continue to have symptoms after taking a proton pump inhibitor. It can also be used to monitor how well treatment is going. Manometry: Involves swallowing a tube that measures the pressure of esophageal muscle contractions. This can help determine if the lower esophageal sphincter is working properly. This test is needed if you have chest pain and/or difficulty swallowing but your upper endoscopy results are normal; this can help rule out motility disorders (problems with how the muscles in the digestive tract work to digest food).

Nội soi cho phép bác sĩ kiểm tra trực tiếp đường tiêu hóa trên nhằm kiểm tra tình trạng bệnh
5. Complications of Gastroesophageal Reflux Disease (GERD)
Most people with GERD will have no serious complications, especially if treated. However, potentially serious complications can sometimes occur in people with severe GERD.Erosive esophagitis: When the esophagus is damaged (eroded) as a result of stomach acid exposure. This can lead to ulcers and bleeding. Bleeding from ulcers is not always visible, which can be detected with a stool test. Esophageal spasm: Acid damage can cause the esophagus to become scarred and narrow, causing a blockage that can cause food or medicine to get stuck in the esophagus. The narrowing is caused by scar tissue that develops as sores that repeatedly damage and then heal in the esophagus. Barrett's esophagus: Occurs when normal cells in the lower esophagus (called squamous cells) are replaced by another type of cell (called enterocytes). This process is often the result of repeated damage to the lining of the esophagus caused by persistent GERD. Intestinal cells are at risk of mutating into cancer cells over time. Therefore, people with Barrett's esophagus are advised to have periodic endoscopy to watch for early warning signs of cancer. Lung and throat problems: If stomach acid backs up into the throat, this can cause vocal cord inflammation, sore throat, or a hoarse voice. Acid can also be inhaled into the lungs and cause symptoms of pneumonia or asthma. Over time, acid in the lungs can lead to permanent lung damage. Dental problems: Repeated episodes of acid reflux can wear down tooth enamel over time.

Các đợt trào ngược axit lặp đi lặp lại có thể làm mòn men răng theo thời gian
6. Treatment of Gastroesophageal Reflux Disease (GERD)
GERD is treated according to the frequency and severity of symptoms and complications.Lifestyle changes: Certain lifestyle and dietary changes can often help reduce the symptoms of GERD. If you have mild symptoms, you can try these methods before seeking medical attention. If your symptoms are more severe, you should talk to your doctor so they can advise.
The following lifestyle changes are generally recommended:
Lose weight (if you are overweight): Losing weight can help people who are overweight reduce acid reflux. In addition, weight loss has a number of other health benefits, including a reduced risk of type 2 diabetes and heart disease. Elevate the head of the bed 15-20cm - Although most people only experience heartburn for a period of two to three hours after a meal, some people wake up at night with heartburn. People with heartburn at night can raise the head of their bed, making the head and shoulders higher than the stomach, gravity will prevent acid reflux. You can raise the head of the bed by placing wooden blocks under the feet or a foam wedge under the mattress. Several companies have developed commercial products for this purpose. However, it is not helpful to add extra pillows; this can cause an unnatural bend in the body that increases pressure on the stomach, which can worsen acid reflux. Avoid foods that trigger GERD symptoms: Some foods also relax the lower esophageal sphincter, which can lead to acid reflux. Taking too much caffeine, chocolate, alcohol, mint, and fatty foods can cause unpleasant acid reflux in some people. It is advisable to limit your intake of these foods when you notice that your symptoms are worse after you have eaten certain of these foods or beverages. Quit smoking: Saliva helps neutralize acid reflux, and smoking reduces the amount of saliva in the mouth and throat. Smoking also reduces pressure in the lower esophageal sphincter and causes coughing, which causes frequent acid reflux in the esophagus. Quitting smoking can reduce or eliminate mild reflux symptoms. Although the evidence is limited, other changes sometimes also seem to help, such as:
Avoiding late meals: Going to bed with a full stomach may increase the risk of acid reflux. Eat at least two to three hours before bedtime, symptoms may reduce. Wear loose, comfortable clothing - tight clothing can increase discomfort, increase pressure in the abdomen, and push stomach contents into the esophagus. 6.1 Treatment of mild GERD In addition to lifestyle changes, initial treatment of mild GERD includes the use of over-the-counter antacids or histamine receptor antagonists.

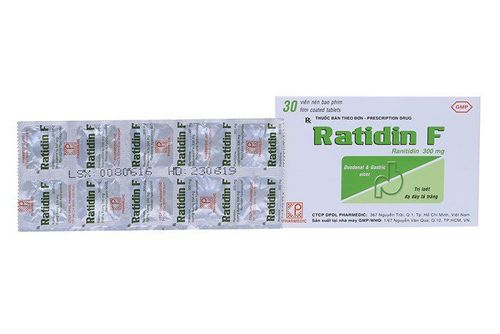
Ngoài thay đổi lối sống, điều trị ban đầu của bệnh GERD nhẹ bao gồm sử dụng thuốc kháng axit không kê đơn hoặc thuốc đối kháng thụ thể histamin
Once your doctor determines the optimal dose and type of PPI for you, you will likely continue to take it for about eight weeks. Most patients no longer have symptoms of GERD after stopping PPIs. Further treatment when the patient's symptoms return.
If symptoms recur within three months of stopping the drug or if you have severe esophagitis, long-term treatment is usually recommended. Your doctor may also recommend an upper endoscopy (if you haven't already) to rule out other problems. If symptoms recur three months or more after stopping the medication, your doctor may recommend another course of PPI therapy. The goal is to take the lowest possible dose of medication to control symptoms and prevent complications. PPIs are safe drugs. However, long-term use of PPIs may increase the risk of certain intestinal infections or decrease absorption of minerals and nutrients. In general, although this risk is very small, it is still necessary to use the lowest effective dose for the shortest time. In addition, the use of PPIs such as omeprazole or esomeprazole (Nexium) has a risk of drug interactions that reduce the effects of cardiovascular drugs (clopidogrel) that can affect cardiovascular diseases (US FDA). If symptoms do not improve: In some patients, symptoms do not completely resolve with PPI treatment. Doctors call this treatment-resistant GERD. If you continue to have bothersome symptoms after a course of PPI treatment, your doctor may:
Divide your PPI dose into 2 (instead of one larger dose per day) Increase your PPI dose or switch to another PPI. The study showed that rabeprazole (Pariet) significantly improved GERD in patients reporting non-responders to previous PPIs from day 1 (>50%) and after 8 weeks (>80%) (Robinson, 2002). Add other medicines: such as prokinetics (Gasmotin), gaviscon,... More testing to confirm the diagnosis of GERD and/or rule out other problems. Consider surgical treatment (see 'Surgical treatment' section below) Treatment of GERD during pregnancy: Treatment of GERD during pregnancy begins with lifestyle changes. If not, your doctor may suggest an antacid followed by a medicine called sucralfate if symptoms persist. It's important to talk to your doctor before trying any over-the-counter medications, as some drugs (including some antacids) are not safe to use during pregnancy.

Điều trị GERD khi mang thai bắt đầu bằng thay đổi lối sống
Surgical treatment: Because lifestyle changes and medications are very effective in controlling GERD symptoms in most cases, surgical treatment has a limited role in GERD. However, it may be an option for some people whose symptoms are not adequately controlled with other treatments, or who are unable to adhere to a medication regimen. Reflux surgery includes repairing a hiatal hernia (if present) and strengthening the lower esophageal sphincter. The most common surgical procedure is the Nissen surgery. This procedure involves wrapping the upper part of the stomach around the lower end of the esophagus.
After Nissen surgery, most people experience symptoms including difficulty swallowing and a feeling of bloating. These symptoms usually resolve with time, but may also persist. There are also other risks associated with surgery. Even so, most people are satisfied with the long-term results of surgery. There are other surgical procedures sometimes used to treat GERD, including less invasive options.
Vinmec International General Hospital with a system of modern facilities, medical equipment and a team of experts and doctors with many years of experience in medical examination and treatment, patients can rest assured to visit examination and treatment at the Hospital.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
ReferencesUptodate: Peter J Kahrilas et al. Gastroesophageal reflux disease in adults. updated: Apr 06, 2020.
Robinson M. et al. Onset of symptom relief with rabeprazole: a community-based, open-label assessment of patients with erosive oesophagitis. Aliment Pharmacol Ther. 2002; 16: 445-454
SEE ALSO
Laparoscopic surgery to create an anti-gastroesophageal reflux valve Learn about robotic surgery for gastroesophageal reflux disease at Vinmec Surgery to treat true gastroesophageal reflux Manager: What you need to know