This is an automatically translated article.
The article was made by doctors of Laboratory Department - Vinmec Central Park International General HospitalThe no-culture technique does not require bacteria to multiply prior to detection. Because bacteriology in medicine has been synonymous with culture of bacteria from patient specimens.
1. Non-implantation technique for diagnosing infection
The culture technique is highly concentrated and has a slow response time because bacterial multiplication is essential, but has limited evaluation and performance because it depends on the bacteria being isolated. or not.
Under the right conditions, some bacteria can be grown in artificial media, and live bacteria may need different needs to grow from patient specimens and those of patients being treated. antibiotic treatment. The no-culture technique does not require bacterial multiplication prior to detection. Some techniques, such as microscopy and the detection of bacterial antigens in the specimen. It can provide quick results, for example with after 2 hours. Other non-implantation methods such as DNA exploration and the application of DNA by PCR amplification.
2. Non-inoculation techniques in the laboratory
2.1 Microscopy Microscopy is an important first step in the examination of all patient samples. The use of the microscope plays a key role in bacteriology. Because bacteria vary greatly in size, too small to be seen with the naked eye, a microscope (KHV) is an essential tool in bacteriology. Microscopes often use visible light as a light source, allowing very small specimens and some structural details to be observed. The total magnification of a specimen can be calculated by multiplying the magnification of the objective by the magnification of the eyepiece. A general rule of thumb for microscopes is that the shorter the wavelength of light used, the higher the resolution. The white light used in fluorescence microscopy has a rather long wavelength and thus structures smaller than 0.2 μm cannot be seen. Electron microscopy can improve this to about 0.001 mm.

Kính hiển vi giúp phóng đại mẫu bệnh phẩm được sử dụng trong xét nghiệm vi sinh
Light microscopy is often used for direct and post-inoculation examination of specimens, such as microscopy and staining. Fresh smears are commonly used to look for:
Blood cells (HC) and to look for bacteria in fluid specimens such as urine, feces or cerebrospinal fluid (CSF). Cysts, eggs and parasites in feces. Skin fungi Protozoa in blood and tissues. For live bacteria it is possible to observe their mobility.
2.2 Staining Staining is usually the staining of cells so that they are easier to see, staining usually dries the material with heat or alcohol mounted on a glass plate for microscopy. Specimens from patient specimens or homogenized by culture and then stained with bacteria. Normally, light rays will pass through a single medium, after dyeing the light will pass through two materials of the specimen and of the medium with different refractive indices, so the light rays will change direction (refraction). at the specimen boundary and increases the contrast between the specimen and the environment. As light rays leave the specimen, they will radiate to very close resolution points on the image, which will enter the objective and the image will be magnified. This specimen can be stored for later observation under a normal light microscope with an oil objective, although this is to preserve the direction of the rays at the highest magnification. The oil will have the same refractive index as the glass slide such that the oil drop will become an optical part of the microscope.
2.3 Gram Staining The most important difference of staining techniques in bacteria is Gram staining: Different staining produces the real miracle that is the cell with different staining properties and based on its reactivity. Gram-staining of bacteria and divided into two main groups:
Gram-positive (violet staining bacteria) Gram-negative (bacteria staining pink) This difference is related to the difference in the structure of the cell wall bacterial cells of two groups.

Tiêu bản cầu khuẩn nhuộm bắt màu Gram dương
2.4 Ziehl-Neelsen staining Ziehl-Neelsen staining for the detection of tuberculosis : Some bacteria and bacteria have a waxy cell wall that cannot be stained like gram stain but must be stained with a special method to detect its presence. Ziehl-Neelsen staining is a dyeing method that uses heat to attach fuchsin to cells and then bleach; Staining of tuberculosis bacteria with fuchsin resists staining with acids and alcohols. In addition, fluorescence staining with auramine, which has a strong affinity for the waxy substance of the cell wall of TB bacteria, can be observed under a fluorescence microscope.
Another staining technique that can be used to detect cell-specific features is single staining. This method is often used to investigate the presence of Corynebacteria or not because this method stains bacteria and discolored particles present in bacteria. Features to aid identification include seed-stored polyphosphates of Corynebacterium spp and lipids in Bacillus spp.
2.5 Black-background microscope Used to observe cell phones and delicate cells like Spirochetes : Microscopes can often be inserted by altering the condenser system so that glare appears against the black background. . Live bacteria can be examined by a black background microscope and can be observed mobile. This method is also used to view very thin cells such as Spirochetes because the light reflected from the surface of the cell makes it appear large and therefore easier to see when viewed with a conventional microscope.
2.6 Phase Contrast Microscopy Phase Contrast Microscopy increases the contrast of an image of an object:
This technique further improves upon very small differences in refractive index and intercellular density Live and their solutions are suspensions so that it produces an image of an object with a higher degree of contrast than is achieved by bright area microscopy. However, phase-contrast microscopy is now rarely used in laboratory diagnosis.
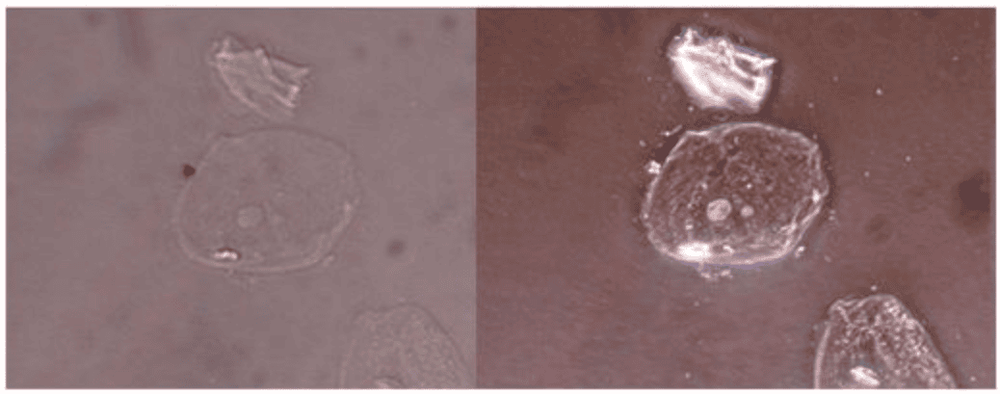
Ảnh chụp tế bào kính hiển vi trường sáng truyền thống và kính hiển vi tương phản
2.7 Fluorescence Microscopy If light of that wavelength shines on an object that fluoresces, it emits light at different wavelengths. Some biological materials naturally fluoresce; Others can be stained with fluorescent dyes and observed under a microscope with a source of ultraviolet light even though of white light.
Fluorescence microscopy, widely used in bacteriology and immunology, has been developed to detect bacterial antigens in test samples and tissues by staining with a specific antibody bound to the dye ( immunofluorescence). This method can be more sensitive or can be attached to detect antibodies by isotope marking a second antibody in the direct test.
2.8 Electron Microscopy The specimen should be sliced; Electron microscopes use an electron beam instead of the lenses used in conventional light microscopes. The system is safe because it works under high vacuum. The electron beam penetrates little and the single bacterial cell is too thick to observe directly. Make this part of the test piece fixed and framed on the plastic and cut a thin section for individual inspection. Eclectron-dense stains such as osmium tetroxide, uranyl acetate or glutaraldehyde for test samples to improve contrast. The electron beam penetrates the cross-section and creates an image of an object on the fluorescent film. The image of an object is photographic and magnified so that the original specimen is magnified by 1000.
Electron microscopy can be used to detect viral molecules: Direct view of the specimen allows rapid identification virus molecules and detect viruses that cannot be cultured such as Rotaviruses, Hepatis A virus. The fluid for viewing must be dried on a copper tube system and observed. About a billion virus molecules in a milliliter are needed if they are to be detectable. Susceptibility may be increased because the fluid is reacting with antiviral antibodies so that viral particles cluster together in visible clusters. It is known as immunoelectron microscopy which is a technique similar to conventional immunofluorescence microscopy.

Hình ảnh kính hiển vi điện tử
2.9 Bacterial Antigen Detection in Specimen Bacterial specific antigen detection could be a faster method to detect the presence of bacteria from the growth and identification of bacteria.
Methods include:
Detection of antigen by its interaction with specific antibodies Detection of bacterial toxins. The specific antibody that coats the latex molecule reacts with the bacteria or its product, resulting in visible clusters. Example: The common causative agents of bacterial meningitis, Streptococcus pneumoniae, Haemophilus influenzae, and Neisseria meningitidis types A and C can be detected in CSF by mixing the specimen with specific fecal-coated antibodies. latex particles. If antigens such as bacteria or by-products are produced and the presence of specific particles will cluster together. This test produces results within minutes of specimen receipt, but its susceptibility is not more important than gram staining and a weak positivity can result from cross-reactive antigens. However, it can be used as a diagnostic aid when the patient is on antibiotic therapy and the bacteria may appear atypically in the CSF and grow weakly in culture.













