This is an automatically translated article.
Post by Master, Doctor Mai Vien Phuong - Gastrointestinal Endoscopy - Department of Medical Examination & Internal Medicine - Vinmec Central Park International General Hospital.The immune system plays a central role in the pathogenesis of inflammatory bowel disease. Hematopoietic stem cell transplantation or solid organ transplantation is performed with the use of steroids and immunomodulators. These agents block an immunogenic response in the recipient's lymphocytes against the transplanted leukocyte antigens.
1. What is secondary inflammatory bowel disease?
Inflammatory bowel disease is a chronic disease of the gastrointestinal tract without a clearly defined etiology and is traditionally referred to as primary inflammatory bowel disease. The currently known factors likely to cause secondary inflammatory bowel disease are medications; surgery to change the gut and transplant organs, stem cells or the fecal microbiota.
After solid organ or hematopoietic stem cell transplantation, recipients may experience flare-ups of inflammatory bowel disease or new-onset inflammatory bowel disease. Fecal microbiota transplantation has been widely used to treat patients with recurrent Clostridium difficile infections but can also cause flare-ups of inflammatory bowel disease.
The diagnosis of inflammatory bowel disease is made by comparing the clinical manifestations, endoscopic findings and histopathological features of the diseased tissue samples. There is no single test to diagnose inflammatory bowel disease or to differentiate between Crohn's disease and ulcerative colitis. Although the use of anti-neutrophil antibodies and anti-saccharomyces cerevisiae antibody titers can sometimes be helpful in differentiating the two.
2. New-onset inflammatory bowel disease after organ transplant surgery The immune system plays a central role in the pathogenesis of inflammatory bowel disease. Hematopoietic stem cell transplantation (HSCT) or solid organ transplantation (solid organ transplantation) is performed with the use of steroids and immunomodulators. These agents suppress the immunogenic response in the recipient's lymphocytes against the transplanted leukocyte antigens, preventing immune-mediated rejection from occurring. Therefore, proper cross-matching is performed prior to transplantation to prevent human leukocyte antigen mismatch.
Alterations in the immune system with the use of immunosuppressants or the introduction of foreign antigens can lead to an upregulated immune response and subsequent development of autoimmune disorders. One such autoimmune condition is inflammatory bowel disease that can develop after HSCT or solid organ transplantation. Another type of transplant is healthy donor fecal material, which is used to treat people with recurrent Clostridium difficile infections. If a donor has inflammatory bowel disease, their gut microbiota may carry an inflammatory microbiome and lead to the development of new-onset inflammatory bowel disease in the recipient. In addition, alterations in the gut microbiota may induce an excessive immune response to newly introduced bacteria, which can lead to immune-mediated intestinal inflammation.

Colon biopsy showed chronic active colitis with granulomatous granulomatosis and the disease may involve the upper or lower gastrointestinal tract, a pattern resembling Crohn's disease. They also tend to have a lot of Bradyrhizobium enterica bacteria in their gut. Some speculate that alterations in the gut microbiota play a role in the pathogenesis of this disease. This is also supported by the fact that antibiotic therapy is effective in treatment. Umbilical cord colitis may be a variant of inflammatory bowel disease that develops in an altered immune environment due to the use of cord blood stem cells or the use of immunomodulatory drugs.
4. Inflammatory bowel disease after solid organ transplantation People undergoing solid organ transplantation are immunosuppressed during the transplant cycle and post-transplant. There is an increased risk of developing diarrhea after transplantation, usually from an infection or as a side effect of medication, but there are other conditions that can cause diarrhea in these patients. Those two conditions trigger flare-ups of inflammatory bowel disease in people with a pre-existing diagnosis of inflammatory bowel disease or the development of new-onset inflammatory bowel disease. This phenomenon is more common after direct liver transplantation than with other solid organ transplants, such as kidney or heart.
Inflammatory bowel disease in general and ulcerative colitis in particular are associated with concomitant primary sclerosing cholangitis, for which the main treatment is direct liver transplantation. This is probably the reason for the higher number of direct liver transplants than solid organ transplants of other organs in the inflammatory bowel disease population. The incidence rates of developing new-onset inflammatory bowel disease in solid organ transplant recipients compared with the general population are 206 and 20 per 100,000 person-years, respectively.
In a study of people after a kidney transplant, it was found that the risk of inflammatory bowel disease was twice as high compared to the general population. In a retrospective histogram review of 6800 liver and/or kidney transplant recipients who received some form of immunosuppression, it was found that 14 developed new-onset inflammatory bowel disease. Post-liver transplant patients who directly develop new-onset inflammatory bowel disease are more likely to develop primary sclerosing cholangitis or to develop primary sclerosing cholangitis in the future.
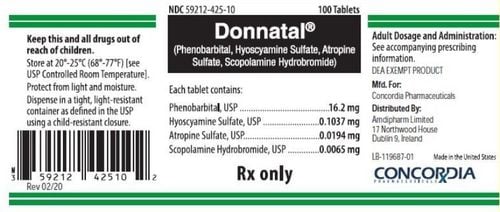
5. Transplant immunosuppressants may be beneficial in patients with posttransplant inflammatory bowel disease intestine. In a study of 41 inflammatory bowel disease patients who underwent direct liver transplantation, clinical remission rates were higher than 42 inflammatory bowel disease patients who did not undergo direct liver transplantation (54% vs 33%, P = 0.03). Transplant recipients who received MMF (mycophenolate mofetil) had better outcomes than those who received other immunosuppressants. This altered response to immunotherapy by different individuals illustrates the complex nature of the immunological processes at play when alterations in immunity cause disease flare-ups in some individuals. when in others it can protect from flare-ups. One could argue that transplant recipients are more closely monitored and more compliant with their medications, thus having less disease flare-ups.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
References: Ghouri YA, Tahan V, Shen B. Secondary causes of inflammatory bowel diseases. World J Gastroenterol 2020; 26(28): 3998-4017 [PMID: 32821067 DOI: 10.3748/wjg.v26.i28.3998]