This is an automatically translated article.
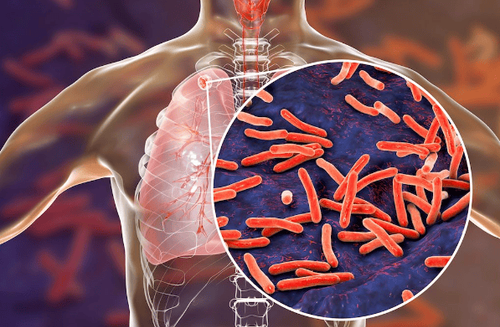
The article was written by MSc Vu Duy Dung - Department of General Internal Medicine - Vinmec Times City International HospitalTuberculosis and HIV/AIDS constitute a large burden of infections in under-resourced countries. In the patient's body, these two pathogens, TB bacteria and HIV virus, promote each other to accelerate the decline of immune function and lead to death if left untreated.
1. Epidemiology of TB/HIV . co-infection
An estimated 14 million people worldwide are co-infected with HIV and TB bacteria, and it is estimated that TB remains the leading cause of death among people living with HIV. HIV infection is estimated to increase the risk of TB by 20-fold compared with people without HIV in countries with high HIV prevalence.
Of the estimated 8.7 million people with TB globally in 2012, approximately 1.1 million (13%) are estimated to have HIV co-infection. Of the 2.8 million people with TB who were screened for HIV in 2012, 20% were HIV-positive. It is estimated that more than 75% of HIV-positive TB cases live in 10 countries (Ethiopia, India, Kenya, Mozambique, Nigeria, South Africa, the Republic of Tanzania, Uganda, Zambia, and Zimbabwe).
The increased prevalence of active TB in people with HIV may be due to at least two mechanisms: increased reactivation of latent TB and increased susceptibility to TB infection.
2. Risk of nervous system damage in people co-infected with HIV/TB
More than 50% of people coinfected with HIV/TB have extrapulmonary TB, and HIV-positive individuals are five times more likely to develop central nervous system damage during TB infection than HIV-negative individuals.
In addition, paradoxical growth of intracranial tuberculosis has been reported in patients appropriately treated with antituberculosis and antiretroviral agents.
HIV infection also increases the risk for both acquired TB and progression from latent to active TB. For patients with advanced HIV infection, high-potency antiretroviral therapy (HAART) reduces the risk for both acquired and advanced TB as well as the prevalence of opportunistic infections and dead.
Because of the higher likelihood of contracting TB in the setting of HIV co-infection as well as the association between HIV infection and poor TB outcomes, HIV testing should be performed in all patients diagnosed with TB.
3. Immune Reconstructive Inflammatory Syndrome (IRIS)
Immune remodeling inflammatory syndrome (IRIS) is an inflammatory response to a previous or undiagnosed infection that may be seen in HIV-infected patients shortly after initiation of HAART. IRIS causes two distinct clinical syndromes: unmasking and paradoxical. Both syndromes responded well to steroids, but IRIS unmasked the need for additional treatment of the underlying infection.
Unmasked IRIS occurs when an occult infection that previously caused no symptoms or signs is recognized by the slowly recovering host's immune system during the first months of HAART. Paradoxical IRIS is the recurrence of inflammation against a previously treated infection by recognition of antigens by the host immune system recovering from HAART; this can occur in the setting of only a small number or no live microorganisms, and cultures are usually negative.
IRIS occurs most commonly in adults, with 17% to 32% of adults having IRIS after initiation of HAART. Approximately 18% of TB patients with HIV infection and initiation of HAART will develop IRIS. Tuberculosis-associated IRIS most commonly presents as fever with clinical exacerbation of lymphadenopathy (in 70%) or respiratory disease (in 30%).
Mycobacterial infections associated with IRIS commonly occur in patients with a mean CD4+ count less than 50 cells/mm3 and a median of 4 weeks after initiation of HAART.
Along with Mycobacterium strains, many other pathogenic microorganisms are associated with IRIS; where neurologists are concerned with cytomegalovirus, Cryptococcus neoformans, varicella-zoster virus, and Toxoplasma gondii.
4. Clinical management of HIV-infected TB patients, including IRIS
Management of HIV-infected TB patients includes effective anti-tuberculosis therapy, concurrent use of antiretroviral therapy (ART), prevention of HIV-related comorbidities, management of HIV toxicity. drugs and prevention/treatment of IRIS.
Treatment of TB in people co-infected with HIV generally follows the same principles as those without HIV. However, caution should be exercised because of interactions between anti-tuberculosis and antiretroviral agents, such as protease inhibitors, and rifamycins, especially rifampicin.
In mild cases of IRIS, specific treatment for IRIS is usually not necessary, but continued treatment with both anti-TB and anti-HIV. If symptoms of IRIS are more evident, high-dose corticosteroids are indicated, particularly for CNS IRIS.
Vinmec International General Hospital is one of the hospitals that not only ensures professional quality with a team of leading medical doctors, a system of modern equipment and technology. The hospital provides comprehensive and professional medical examination, consultation and treatment services, with a civilized, polite, safe and sterile medical examination and treatment space. Customers when choosing to perform tests here can be completely assured of the accuracy of test results.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.














