This is an automatically translated article.
This article is professionally consulted by Master, Resident Doctor Dang Thi Ngoan - Pediatrician - Neonatologist - Department of Pediatrics - Neonatology - Vinmec Ha Long International Hospital.Meningococcal meningitis is a dangerous disease with high mortality and sequelae, especially neonatal purulent meningitis. Therefore, it is necessary to periodically examine to detect neurological sequelae and have timely treatment.
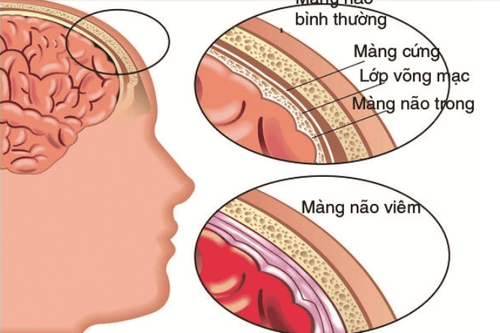
1. What is purulent meningitis?
Meningitis is a bacterial infection of the meninges caused by pathogens capable of producing pus, mainly some bacteria that invade the meninges. This is a common disease in children, especially children under 5 years old, with high mortality and sequelae.
3 most common bacteria causing meningitis are: Streptococcus pneumoniae; H. influenza (Haemophilus influenza) and meningococcal (Neisseria meningitidis). Particularly in infants, the common bacteria causing meningitis are B.streptococcus, Escherichia coli, Listeria monocytogenes. In addition, some other bacteria and fungi can also be the cause of purulent meningitis but are less common and often occur in patients with immunocompromised conditions, sepsis,...
2. Symptoms of purulent meningitis in infants
The clinical presentation of pediatric patients with purulent meningitis is often a combination of fever, irritability, or lethargy. The disease is common in premature babies, amniotic infections, and postpartum asphyxia. Specific symptoms include:
Infection syndrome is often not obvious, there may be no fever, even hypothermia, crying or lethargic child, fatigue, poor feeding, pale skin; Meningeal syndrome incomplete or insidious presentation. The infant often refuses to feed, vomits, groans, has irregular or stopped breathing, bulging or distended fontanel, abdominal distension, diarrhea, decreased muscle tone, loss of neonatal physiological reflexes and possibly convulsions.

Biểu hiện lâm sàng của viêm màng não mủ ở nhi là sốt li bì
3. Diagnostic tests for meningitis in infants
Test of cerebrospinal fluid: is the most important test, decisive for definite diagnosis. Pediatric patients should have a lumbar puncture as soon as clinical examination is suspected of meningitis. The patient's cerebrospinal fluid is cloudy like young coconut water, rice water or pus. When examining or cultured cerebrospinal fluid will identify the bacteria causing the disease. The biochemical test of cerebrospinal fluid can detect high protein concentration (usually above 1g/l), glucose drop below 2.2mmol/l, high cell count (from several hundred to thousands/mm3), in which white blood cells neutral multicore demand predominates; Blood count: Usually, white blood cells are elevated, neutrophils predominate, and hemoglobin levels decrease (anemia); Blood culture and pharyngeal fluid culture, aspirate at the hemorrhagic necrosis, ... help identify pathogenic bacteria; Computed tomography of the brain, trans- fontanelle ultrasound,... to identify possible complications; Cerebrospinal fluid tests help in differential diagnosis of atypical pyelonephritis such as PCR, specific ELISA,...; Electrolyte test, blood gas, ... to support comprehensive treatment.
4. Complications and sequelae of purulent meningitis
4.1 Complications
Injury to cranial nerves: cords II, III, IV, VI, VII, VIII,...; Brain abscess, subdural abscess, pus accumulation along blood vessels, thrombophlebitis, inflammation around cerebral blood vessels,...; CSF blockage and thickening of meninges, obstructing CSF circulation, hydrocephalus syndrome; Extra-nervous system complications depending on bacterial etiology, such as: toxic shock, visceral bleeding (seen in sepsis, meningococcal meningitis), arthritis, nephritis, endocarditis , pericarditis, pneumonia,... 4.2 Sequelae
After purulent meningitis, cases of late diagnosis and treatment may experience the following sequelae:
Strabismus, mute, deaf, blindness, hydrocephalus syndrome,...; Localized nerve damage causing paralysis: Paralysis of 1 limb, hemiplegia, paralysis of 2 lower limbs, cranial nerve damage,...; Memory loss, dementia, mental disorders,...; Epileptic. 4.3 Mortality
The average mortality rate in patients with meningitis is 7 - 10% (due to meningococcal disease), 30% (due to pneumococcal disease) and 10 - 14% (due to H. Influenzae). Early deaths due to respiratory failure, severe cerebral edema, irreversible shock,... Late death due to complications of severe brain and extracerebral infections including brain abscess, nephritis, pneumonia, extensive ulcers and exhaustion, a state of prolonged brain loss leading to brain failure,...

Viêm màng não mủ gây ra nhiều di chứng nghiêm trọng
5. Treatment of neonatal purulent meningitis
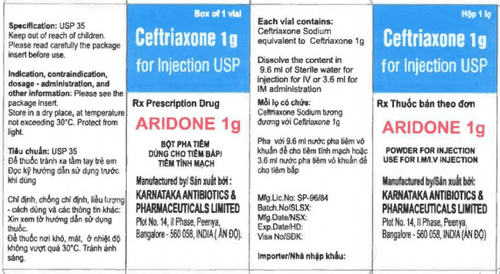
5.1 Use of antibiotics
When the cause is unknown, combine treatment with 2 antibiotics: Ampicillin at a dose of 100mg/kg/24 hours and Gentamicin at a dose of 5mg/kg/24 hours; 48 hours after the second lumbar puncture, if the cerebrospinal fluid is better, the clinical picture is better, continue using the antibiotics used. If cerebrospinal fluid worsens, clinical symptoms do not improve, change antibiotics: Rocephin 80mg/kg/24 hours with amikacin 15mg/kg/24 hours or acepim 80mg/kg/hour with amikacin dose 15mg/kg/24 hours; When there are results of antibiogram: Treatment according to antibiogram, antibiotic treatment duration of 21 days, number of times of pre-cerebrospinal examination should be limited to the lowest level. 5.2 Supportive treatment
Respiratory and circulatory support; Fully nourished; Anti-convulsant; Fight brain edema by lying with your head at 30o high, limit water, the amount of fluid put into the body is equal to 1⁄2 - 2/3 of the need; Correction of acid-base electrolyte balance. 5.3 Follow-up and re-examination
Monitor the baby's head and chest circumference daily; Re-examination every 3 months to detect neurological sequelae. Neonatal purulent meningitis can cause many dangerous neurological sequelae. Therefore, after the treatment is cured, parents need to take their children to regular check-ups as prescribed by the doctor to detect and have a timely treatment plan if they unfortunately encounter neurological sequelae.
Pediatrics Department at Vinmec International General Hospital has been treating pediatric respiratory and tropical infections, with the following advantages:
Modern and advanced facilities system Dedicated team of doctors with a wealth of experience from leading pediatric hospitals in Vietnam The treatment in a quiet, sterile environment, minimizing external influences helps children recover quickly and reduce hospital stay. for children. Customers can directly go to Vinmec Health System nationwide to be examined, examined and diagnosed by a doctor, or book an appointment online HERE.
Recommended video:
Acute, chronic otitis media causing complications, brain abscess, meningitis
MORE:
Meningitis in children: Causes, symptoms, complications Meningitis pus Meningitis in adults: Causes, symptoms and treatment