This is an automatically translated article.
Article by Pharmacist Nguyen Thi Thanh Nga - Clinical Pharmacist - Faculty of Pharmacy - Vinmec Times City International General Hospital1. The role of Vancomycin's blood drug concentration monitoring activity
Blood Drug Monitoring (TDM) is the clinical practice of quantifying drug levels in the blood at defined intervals, in order to optimize drug dosing regimens. TDM is recommended for drugs with narrow therapeutic ranges, drugs with variable pharmacokinetics, drugs that are difficult to reach target concentrations, drugs with a concentration-effectiveness-side effect relationship. The goal of TDM is to individualize the dosing regimen in order to maximize therapeutic efficacy and reduce adverse drug effects.
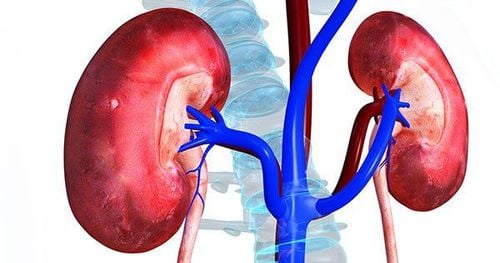
Vancomycin is an antibiotic with a narrow therapeutic range, and this therapeutic range has been narrowing more and more in the last two decades because the susceptibility of bacteria to this antibiotic changes over time, the susceptibility breaking point. The MIC of vancomycin for Staphylococcus aureus was also adjusted from ≤ 4 mg/L to ≤ 2 mg/L. When first introduced in the 1980s, the target vancomycin trough concentration was defined as 5–10 mg/L, but this target was increased to 15–20 mg/L in the 2009 IDSA-ASHP-SIDP recommendation. , to ensure bactericidal effectiveness in the treatment of complicated infections caused by MRSA or the treatment of MRSA strains with MIC = 1 mg/L [5]. On the other hand, as trough concentrations increase, especially when > 15 mg/L, the risk of nephrotoxicity also increases 2.5-fold in pediatric patients and even 3.6-fold in pediatric patients receiving treatment. positive value. Therefore, monitoring of drug levels in the blood is necessary, helping to limit the risk of toxicity, especially vancomycin-related renal events. For some special patient groups, vancomycin pharmacokinetics are highly variable (pediatric patients, critically ill patients, burn patients, ...), monitoring of vancomycin blood concentrations plays a role. important role in the individualization of treatment.
In order to ensure the effectiveness and safety of patients during the use of vancomycin antibiotics, Vinmec Times City Hospital is one of the first hospitals in Vietnam to regularly deploy vancomycin blood concentration monitoring services for patients. both adults and children.

2. Methods of monitoring vamcomycin concentrations in the blood
Vancomycin is a glycopeptide antibiotic that plays an important role in the treatment of serious infections caused by resistant Gram-positive bacteria. As an antibiotic with a narrow therapeutic range, pharmacokinetic parameters highly variable between different patient groups, this antibiotic is recommended for blood drug monitoring (TDM) to individualize the dose for each patient. each patient, ensuring treatment effectiveness as well as patient safety. The practice guidelines for vancomycin TDM have varied over time and the recommended TDM methods are as follows:2.1 TDM vancomycin by trough concentration (Ctrough) Pharmacokinetic, pharmacodynamic (PK/PD) parameters ) have been proposed as a monitoring parameter for vancomycin treatment, including T > MIC (time greater than MIC), AUC/MIC (ratio of area under the curve to inhibitory concentration). minimum), or Cmax/MIC (ratio of peak concentration to minimum inhibitory concentration). Based on animal models, AUC/MIC was determined to best reflect vancomycin's bactericidal efficacy against Staphylococcus aureus, including MSSA, MRSA, and resistant Staphylococcus aureus strains. intermediary (VISA).
Moise-Broder et al. proposed a target AUC/MIC ≥ 400 to ensure the bactericidal effect of vancomycin [15]. However, quantification of multiple concentrations of vancomycin to calculate AUC is difficult in clinical practice, so trough concentration (Ctrough) has been chosen as a proxy for AUC and is recommended in the guidelines for AUC. IDSA-ASHP-SIDP's Vancomycin Treatment Monitor in 2009. In the following years, many institutions also released guidelines for monitoring blood levels of vancomycin based on this 2009 consensus [26].
2.2 Recommendations for the quantification of vancomycin trough concentrations The Ctrough sample is recommended to be obtained immediately before the next infusion of the next dose at equilibrium (possibly immediately before the 4th dose). This concentration is recommended to be ≥ 10 mg/L to limit the development of antibiotic-resistant bacteria. For complicated infections (bacteremia, endocarditis, osteomyelitis, meningitis, hospital-acquired pneumonia), a target Ctrough concentration of 15-20 mg/L is recommended to increase the likelihood of infection. ability to penetrate the organization and optimize treatment effectiveness, this is also the target proposed in many guidelines around the world before 2020. However, these recommendations are mainly based on research data from adults. . In children, the trough range of 10-20 mg/L is difficult to achieve, even though a dose of 60 mg/kg/day has been used. Eiland's study on pediatric patients with an average dose of 59mg/kg/day found that only 49% of patients achieved Ctrough concentrations in the range of 10-20mg/L. According to Glover et al., to achieve a mean trough concentration of 7.8 mg/L, intensively treated pediatric patients required an average dose of 60.6 mg/kg/day. Meanwhile, several vancomycin pharmacokinetic studies in children have shown that trough concentrations of 7-10 mg/L alone can help achieve the AUC target in the majority of patients.

Several other authors also published results on Ctrough's predictability of AUC in adult patients, with coefficient of determination R2 ranges from 51% according to Kamel to 73.1% according to Clack. Similar studies in children have also produced very mixed results. While Ploessl (2015) and Regen (2019) reported an unclear correlation between Ctrough and AUC (R2 0.082 and 0.32) respectively, two studies by Suchartlikitwong (2019) and Alsultan (2020) noted the There is a strong correlation between these two parameters in the studied pediatric population (R2 0.94 and 0.82, respectively). However, the method of determining AUC in different studies is different, which may also be an important factor affecting the results of the correlation between these two parameters.
In addition, the use of Ctrough as a monitoring parameter for vancomycin therapy may increase nephrotoxicity. The study by Finch et al found that total vancomycin dose and Ctrough concentrations were higher in the group of patients receiving Ctrough for treatment monitoring compared with the group of patients monitored with AUC. The incidence of nephrotoxicity was also significantly lower in the vancomycin AUC-monitored group than in the Ctrough-monitored group. Furthermore, trough concentrations >15 mg/L were associated with a 3.5-fold increased risk of nephrotoxicity in adults (OR = 3,643; 95% CI [1.749–7.587]) and more than 2.5-fold in children children (OR = 2.51; 95% CI [1.62 – 3.89]).
Because Ctrough is not really a good proxy for AUC and Ctrough treatment monitoring may increase the risk of nephrotoxicity in patients receiving vancomycin, this parameter is no longer recommended as a monitoring parameter. vancomycin concentrations with serious infections due to MRSA in the 2020 updated IDSA-ASHP-PIDS-SIDP guidelines. For non-serious or other infections, there is insufficient evidence to conclude that vancomycin therapy should be monitored according to Ctrough or AUC. However, according to the guidelines of the Chinese Pharmacological Association published in the journal Clinical Infectious Diseases in 2020, Ctrough is still recommended with a strength equivalent to AUC in facilities that do not have the conditions to deploy TDM vancomycin according to the AUC. The Ctrough target in this guideline is 10-15 mg/L in adults, or up to 20 mg/L in patients with severe infections; Ctrough targets in pediatric and neonatal patients are recommended 5–15 mg/L. Dose adjustment is based on the ratio of the Ctrough target to the measured Ctrough.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.