This is an automatically translated article.
Mesenteric artery infarction is a rare vascular emergency with no typical or specific presentation. Therefore, if mesenteric artery infarction is recognized, examined and treated at an early stage, the success rate will be much higher.
1. What is mesenteric artery infarction?
Infarction of the mesenteric artery is a disease caused by the blockage of blood vessels supplying the small intestine and large intestine, which over time will cause bowel necrosis, easily leading to death. The frequency of the disease has not been accurately calculated, but it can be seen in about 0.1 - 0.2% of the total number of hospitalized patients. Accordingly, mesenteric artery infarction is caused by three main causes: thrombosis, embolism or non-obstructive causes.
1.1. Mesenteric artery infarction due to thrombosis
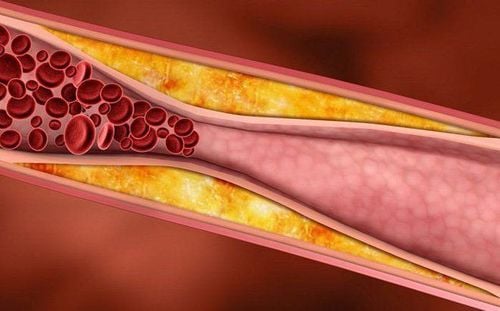
At the sites of narrowing due to severe atherosclerotic plaque, blood clots will form, causing embolism. Most often seen in patients with a history of severe atherosclerosis, including coronary artery disease, cerebrovascular disease and dyslipidemia.
Atherosclerotic plaques are usually slow to progress, so that vascular obstruction is pre-existing and sometimes systemic circulation is present to compensate for the chronic lack of blood supply to the intestinal loops.
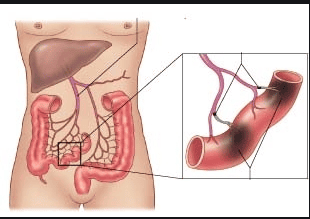
Hình ảnh nhồi máu động mạch mạc treo do huyết khối
1.2. Mesenteric artery infarction due to embolism
Blood clots causing mesenteric artery embolism are transferred from other sites, most of which are thrombus from the heart. Therefore, patients often have a history of cardiovascular disease such as valvular stenosis, valvular regurgitation, left atrial enlargement, atrial fibrillation, or after acute myocardial infarction.
Besides, blood clots causing embolism can also be caused by doctors after coronary stenting procedures, contrast coronary angiography...
Mesenteric artery embolism can only block one Partial or complete occlusion of the artery, is common at sites of spontaneous vascular stenosis, and rarely with pre-existing chronic ischemia.
1.3. Mesenteric artery infarction not due to embolism or thrombosis
Pathology caused by continuous constriction of the mesenteric artery, decreased perfusion and lack of oxygen supply to the intestinal loops leading to necrosis, severe infection. In particular, small blood vessels are constricted more than large blood vessels.
If not diagnosed and intervened quickly, the disease progression will progress from intestinal ischemia to transmucosal infarction, eventually leading to intestinal perforation, peritonitis, and even death.
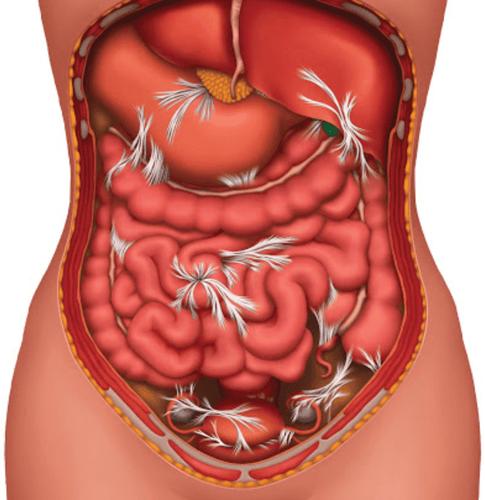
Viêm phúc mạc có thể xảy ra đối với nhồi máu động mạch mạc treo không do thuyên tắc hay huyết khối
2. Clinical signs of mesenteric artery infarction
Manifestations of mesenteric artery infarction are atypical and non-specific, easily misdiagnosed with other intra-abdominal diseases such as: peritonitis, enteritis, gastritis, acute pancreatitis ...
Patient Abdominal pain is severe, but up to 25% of patients do not have abdominal pain. Pain associated with vomiting, diarrhea. This is explained by the fact that when the intestine is ischemic, the first reaction is continuous contractions to expel the contents of the intestinal lumen. Abdominal distension and gastrointestinal bleeding of unknown etiology may be the sole presenting symptom, particularly commonly seen in nonobstructive mesenteric infarction. On physical examination, abdominal compression for tenderness and spasticity may be absent or indistinct in the early stages. The most painful location is the right iliac fossa - the location of the bowel loops that are supplied with blood by the small branches of the mesenteric artery. Late signs of bowel necrosis are more obvious: The patient has high fever, blood in the urine, auscultation, loss of bowel movements and signs of generalized peritonitis.

Đau bụng là triệu chứng của bệnh động mạch mạc treo
3. Subclinical diagnosis of mesenteric artery disease
3.1. Blood tests
The white blood cell count is elevated, the blood lactate and D-Dimer levels are also increased, and the blood tends to have a metabolic acidosis when the intestinal loops are necrotic. However, these blood tests are usually only detected in the late stages and are not valuable in early diagnosis in the stage of bowel without severe necrosis.

Xét nghiệm máu là một trong những phương pháp chẩn đoán
3.2. Unprepared standing abdominal X-ray and general abdominal ultrasound
The above techniques usually give nonspecific results. These imaging studies are mainly used to detect late-stage bowel changes. Includes water-vapor levels in the small intestine, colon, dilated bowel loops, and presence of fluid in the abdomen on radiographs. On ultrasound, the intestinal loops can be seen dilated and filled with fluid, thickening of the small bowel wall and free abdominal fluid.
3.3. Doppler ultrasound of blood vessels
This clinical examination can help detect proximal occlusion of the superior mesenteric artery at an early stage, sometimes the value of Doppler ultrasound is equal to that of angiography if the stenosis is severe or the artery is completely occluded. mesentery.
The advantage of this method is that it is non-invasive, fast and flexible at the bedside. The disadvantage of ultrasound is that the results obtained are highly dependent on the experience of the operator. In particular, when the abdomen is slightly distended due to paralytic ileus, the abdominal examination is also greatly limited.
3.4. Computed tomography CT scan
This is a noninvasive method that can help diagnose mesenteric embolism with a sensitivity of 64-82%, a specificity of 92%. CT features include: thrombus in the mesenteric artery, air in the bowel loops, bowel wall without contrast... However, these signs appear in the late stages of anemia mesentery, when there is already severe intestinal damage such as infarction and necrosis.
Recently, the technique of multi-slice computed tomography combined with three-dimensional reconstruction helps to quickly detect thrombus in the vascular lumen, as well as early lesions of the intestinal mucosa, greatly helping to Early and effective diagnosis and treatment, thereby improving the mortality rate of acute mesenteric embolism

Chụp cắt lớp vi tính CT scan giúp chẩn đoán bệnh
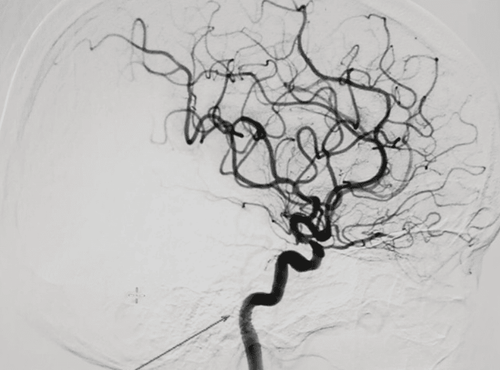
3.5. Angiography
This is the subclinical with the highest diagnostic value for mesenteric artery infarction. This imaging helps to accurately describe the anatomy of the mesenteric artery, find the exact cause of the infarction, but also combine immediate treatment with vasodilator infusion (Papaverin) into the artery selectively or anticholinergic drugs. crowded in some cases.
The limitation of this method is that the procedure is invasive, time consuming, not always possible and the effectiveness of treatment depends on the stage of the disease, when the small intestine has not been necrotic.
4. Treatment of mesenteric artery infarction
If the patient is diagnosed early, when the intestine is not necrotic, treatment with angiography, infusion of a vasodilator (papaverin) directly into the mesenteric artery can help the intestine to recover completely.
Surgery is indicated in cases of mesenteric artery infarction complicated by peritonitis, small bowel infarction or severe infectious necrosis. The purpose of surgery is to help evaluate intestinal ischemia, the ability of the intestine to recover, and to perform resection of the infarcted bowel.
Other treatments include:
Antibiotics if the patient has signs of infection Insertion of a nasogastric tube with continuous suctioning. Vinmec International General Hospital is the address for examination, treatment and prevention of diseases. When performing the examination process at Vinmec, customers will be welcomed and used modern facilities and equipment along with perfect medical services under the guidance and advice of experts. Good doctors, well-trained both at home and abroad.
Customers can directly go to Vinmec Health system nationwide to visit or contact the hotline here for support.