This is an automatically translated article.
Posted by Master, Doctor Mai Vien Phuong - Department of Examination & Internal Medicine - Vinmec Central Park International General Hospital
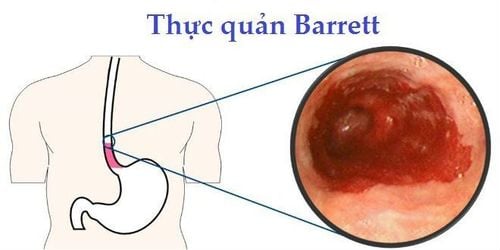
The detection of neoplasms in the diagnosis of Barrett's esophagus (BE) remains challenging because the current gold standard quadrant biopsies have a high miss rate and are poorly followed. Evidence supporting the use of acetic acid (acetic acid C) endoscopic therapy is growing.
1.Mechanism of action of acetic acid in the diagnosis of Barrett's esophagus
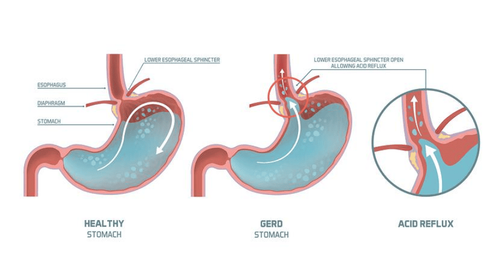
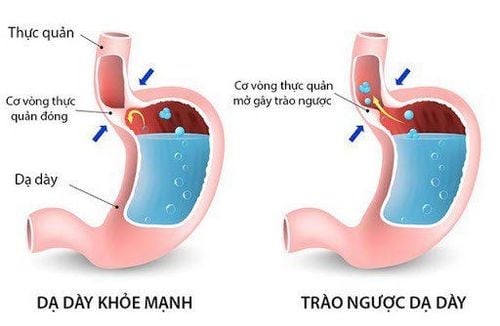
The use of acetic acid (AA) in the gastrointestinal tract was first reported by Guelrud and Herrera, to aid in the identification of islets of Barrett's esophagus following dissection therapy. This technique of gynecological origin, where acetic acid is injected into the cervix has been used to highlight dysplastic areas during cervical endothelial cancer screening. When acetic acid is sprayed onto the squamous epithelium, an acetogenic reaction occurs by masking the submucosal capillaries and increasing the opacity of the mucosal surface. When acetic acid (pH 2.5-3.0) penetrates the multilayered squamous epithelium, it is neutralized, protecting the subepithelial layer and vasculature. In contrast, when sprayed onto Barrett's epithelium, at low concentrations (1%-3%), acetic acid initially removed the superficial mucin layer by disrupting glycoprotein disulphide bonds. The unbuffered acid then induces a reversible acetylation of cytosolic proteins and changes the spatial properties of nuclear and cytoplasmic proteins, initially inducing acetosis that highlights the surface pattern. .
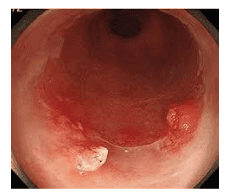
With disruption of the mucus layer, acetic acid reaches the stromal capillaries causing vascular occlusion, resulting in focal erythema but this is hidden under the acetowhite mucosa and appears only after the loss of acetowhitening. Focal erythema due to LAW was first described by the Portsmouth group in 2010, as a strong predictor of neoplasia. The exact mechanism remains unclear but it is believed that the difference in acetowhitening response between noncancerous and cancerous mucosa is due to the difference in nucleocytoplasmic ratios between noncancerous and cancerous cells. The low cytoplasmic content of cancer cells allows them to lose acetone more rapidly than in non-cancerous cells. This reaction leads to focal erythema - a pathological sign of neoplasia with acetic acid.
2.Acid acid for diagnosis of non-proliferative Barrett's esophagus
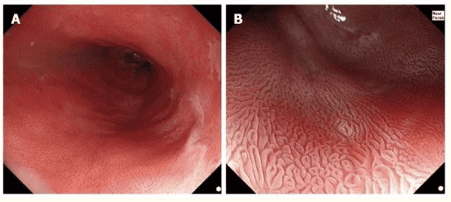
The diagnosis of Barrett's esophagus, according to American society guidelines, is defined as the presence of intestinal metaplasia of the esophagus. Because intestinal metaplasia cannot be easily identified by white light endoscopy, this diagnosis is made on histology. Attempts have been made to visually identify intestinal metaplasia by advanced endoscopy. Acetic acid combined with magnifying endoscopy has been shown to accurately identify intestinal metaplasia. Guelrud et al. classified the surface of Barrett's mucosa into four categories: (1) circular pits; (2) mesh (round or oval pit); (3) villi (appears as fine villi without visible pitting); and (4) ridged (thick villi with complex, brainlike shape without visible pits).
They found that pattern I corresponds to cardia or fundus type without intestinal metaplasia and patterns II, III, IV correspond to intestinal metaplasia with increasing sensitivity. The overall accuracy of acetic acid with magnifying endoscopy for the diagnosis of intestinal metaplasia was 92.2%. These findings have been reliably described by Toyoda et al. and Fortun et al.
3. What do the studies say?
A recent meta-analysis by Coletta et al evaluated the use of acetic acid to detect intestinal metaplasia and high-grade dysplasia/oesophageal adenocarcinoma in patients with Barrett's esophagus by histology. reference standard. A total of 13 prospective studies (1690 patients) were included in the meta-analysis. Eight of the 13 studies, provided data on the diagnosis of intestinal metaplasia. For the characteristics of intestinal metaplasia, the combined sensitivity, specificity, likelihood ratio positive (LR+) and likelihood ratio negative (LR-) for all included studies (8 studies). study, 516 patients) were 0.96 (95% CI: 0.83-0.99) , 0.69 (95% CI: 0.54-0.81), respectively, 3.0 (95 CI: 95). %: 2.0-4.7) and 0.06 (95% CI: 0.01-0.26). No significant sources of heterogeneity were identified in the subgroup analysis.
Acetic acid may be useful to rule out specific intestinal metaplasia, however, histological confirmation is still important due to its low specificity (0.69). In the authors' view, it is not clinically appropriate to manage long-segment Barrett's esophagus because the presence of specific intestinal metaplasia would not alter the duration of surveillance.
4.Acetic acid in the detection and characterization of neoplasia
The use of acetic acid to aid in the identification of intestinal metaplasia in Barrett's esophagus is important in stratifying monitoring intervals. However, the important utility of acetic acid is the identification and characterization of Barrett's neoplasm. There is increasing evidence supporting the use of acetic acid in this environment.
In 2006, Réaud et al., continued Guelrud's study to determine the appearance of Barrett's esophagus neoplasm after 6% acetic acid dye injection and magnified endoscopy. In their study of 28 patients, they noted that those with high-grade dysplasia on biopsy showed mucosal structural disorganization and increased vasculature – a phenomenon identified by Rey et al. earlier in 2003. Using these parameters, they demonstrated a positive predictive value (PPV) of 75% for cancer. Camus et al. identified similar characteristics when combining acetic acid with FICE.
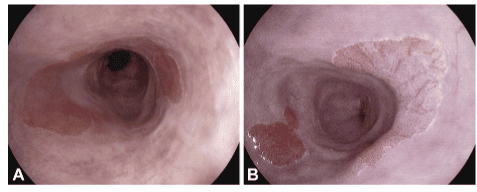
5.Combination of magnifying endoscopy and acetic acid in the diagnosis of patients with Barrett's esophagus
In their study of 62 patients in 2006, Fortun et al tested whether a combination of magnified endoscopy and 3% acetic acid could improve diagnostic accuracy in patients with real Barrett manage or not. Patients with repeat endoscopy recently underwent diagnostic endoscopy (median prior 7 months). Barrett's cancer was identified in 9 patients: 5 low-grade dysplasia, 1 high-grade dysplasia, and 3 esophageal adenocarcinomas. The main limitation of this study is that index endoscopy was used as a control, raising the question of whether the detected tumor was de-novo or previously missed, given the small total tumor count. . Simultaneously, Yagi et al. reported that Barrett's esophageal adenocarcinoma was associated with an irregular granule or small granules after 1.5% acetic acid dye injection and magnified endoscopy.
One year later, Vázquez-Iglesias et al. reported on their prospective study of 100 patients under Barrett's follow-up, 13 of whom had cancer, using 3% acetic acid and unmagnified endoscopy. . They proposed the following mucosal classification: (1) normal pattern: uniform mesh along the entire esophagus with column lined; and (2) irregular pattern: rough or irregular mesh.
Applying these features, they demonstrated 100% sensitivity and 97.7% specificity (PPV 86% NPV 100%) for early cancer detection. With cases of false positives arising in 2 patients; One has esophagitis, the other has an esophageal ulcer.
6.The role of acetic acid is increasingly interested
The advent of advanced endoscopic imaging technologies such as NBI, FICE and i-scan has improved the identification and characterization of cancerous lesions, but these technologies require financial investment. significantly main. Therefore, the role of acetic acid in the diagnostic population is of great interest as a potentially cost-effective, accurate, and non-exclusive tool to improve dysplasia detection.
6. Cost-effectiveness of acetic acid-targeted biopsy procedures
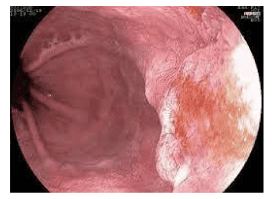
Bhandari et al conducted a retrospective cohort study of all acetic acid procedures for Barrett's esophagus performed between 2005-2010 to examine the effectiveness and cost impact of this approach in cancer identification. This study was conducted in one center with all procedures performed by a single endoscopic specialist. High definition white light endoscopy (HDWL) was used in all cases prior to 2.5% acetic acid. Targeted biopsies of all acetic acid-enhanced visible lesions were performed, followed by random four quadrants. 197 high-risk patients underwent 263 procedures. Of these, 68 patients were diagnosed with high-grade dysplasia not seen at random biopsy. Notably, there was a high incidence of high-risk cancers (high-grade dysplasia/oesophageal adenocarcinoma) in this patient group (143/263 procedures; 54.4%). Cancer detection with acetic acid (96%) was more than twofold compared with HDWL (48%), P = 0.0001 missed high-grade dysplasia with acetic acid in 5/98 patients (5.1%) , however, 4 of these are in the complex, post-EMR follow-up group.
They performed an algorithm that modeled the cost of 3 alternative biopsies that incorporate acetic acid using their median Barrett esophagus length of 4.5cm. The neoplastic tumor missed rate was 4% in the biopsy group that targeted only acetic acid. However, the calculated cost savings are significant in the context of the high-risk population included in this study and if applied to the normally diagnosed population with low cancer incidence. more than <5%, the cost-effectiveness increased by 10 times.
Conclusion The evidence for the use of acetic acid in the detection and characterization of Barrett's cancer is convincing. Large studies from the Portsmouth and Wiesbaden groups demonstrate that experts can meet the ASGE PIVI criteria (sensitivity ≥ 90%, NPV ≥ 98%, and specificity > 80%) and thus be able to differentiate reasonable coordination with four random quadrants. The technique is cheap and widely applicable, independent of the endoscope manufacturer. However, more data from a well-supplied randomized controlled trial are needed before abandoning four quadrants of randomization completely and it is possible that the modified Portsmouth protocol provides optimal results for diagnosis. cost-effective Barrett prediction.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.