This is an automatically translated article.
Articles written by MSc, BS. Nguyen Thuc Vy, Department of Diagnostic Imaging - Vinmec Nha Trang International General Hospital
Diffuse axonal injury is a severe pathology of traumatic brain injury that causes many serious complications. The most optimal imaging method in this case is magnetic resonance imaging (MRI).
1. Introduction
Diffuse axonal injury (DAI) is a type of brain injury caused by traumatic brain injury. Traumatic brain injury can be classified into mild, moderate, or severe based on the Glasgow coma scale. Traumatic brain injury with a Glasgow score of 13-15 points is classified as mild, from 9-12 points is classified as moderate and less than 8 points is classified as severe.
Primary diffuse axonal damage affects white matter pathways in the brain. Clinically, patients with DAI present with a wide range of neurological disturbances that can range from clinically insignificant to comatose state. However, most DAI patients are defined as severe and usually have a Glasgow score of less than 8.
2. Cause
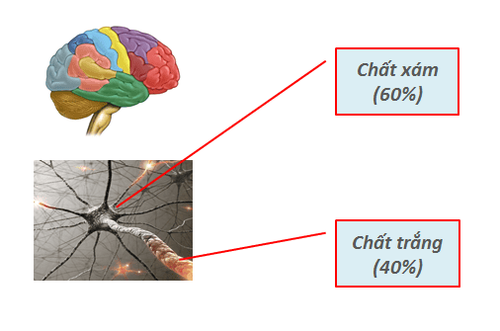
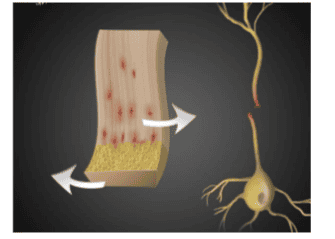
The most common cause of diffuse axle trauma is related to high-speed motor vehicle crashes. The most common mechanism involves accelerated and decelerated motion resulting in shearing of the white matter regions of the brain. This leads to micro- and gross damage to axons in the brain at the border of gray and white matter. Diffuse axial lesions usually affect white matter regions at the white matter–gray matter boundary, involving the corpus callosum and brain stem. Interestingly, there was no association between diffuse axonal injury and skull fracture.

3. Epidemiology
The true incidence of DAI is unknown. However, it is estimated that about 10% of all hospital admissions with traumatic brain injury will have a certain percentage of DAI. Among patients with DAI, an estimated 25% will result in death. Autopsy studies have shown that patients with severe traumatic brain injury have a significant proportion of diffuse axonal damage.
4. Pathology
Diffuse axonal injury (DAI) is usually due to rotational acceleration or sudden deceleration. Due to the different densities of the white and gray matter, a sudden change in velocity leads to axonal shearing/jerking at the gray-white matter junction. In most cases, the forces This leads to cellular damage and edema, and complete axonal rupture is seen only in severe cases. Some nerve cells may degenerate in the weeks or months following an injury, which is called secondary axonotmesis.
Usually, patients with diffuse axial lesions present with bilateral neurologic deficits, usually affecting the frontal and temporal white matter, the corpus callosum, and the brain stem.
Adams classification of diffuse axonal injury using pathophysiological white matter lesions and clinical presentation:
Grade 1: Mild diffuse axonal injury with microscopic white matter changes in cerebral cortex, corpus callosum, and brain stem. Grade 2: Moderately diffuse axonal injury with gross focal lesion in the corpus callosum. Grade 3: Severe diffuse axonal damage with grade 2 findings and focal brainstem lesions.
5. History
DAI is a clinical diagnosis. Typically, DAI is considered in patients with a Glasgow score of less than 8 for more than six hours. The clinical presentation of patients with diffuse axonal injury is related to the severity of the diffuse axonal injury. For example, patients with mild axonal injury have signs and symptoms that reflect concussion. These symptoms often include headache, dizziness, nausea, vomiting, and fatigue. However, patients with severe diffuse axonal damage may also present with loss of consciousness and a persistent vegetative state. A very small number of patients with severe diffuse axial trauma will regain consciousness within the first year of injury.
6. Diagnosis
In general, diffuse axonal injury is a severe form of traumatic brain injury. Patients with head trauma from rotation or deceleration should be suspected of having DAI. In general, DAI is diagnosed after a traumatic brain injury with a GCS of less than 8 for more than six consecutive hours.
DAI imaging:
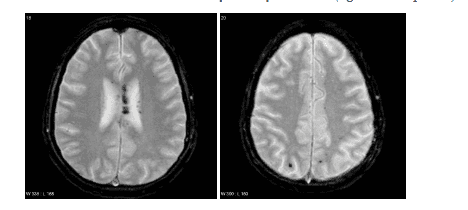
Non-contrast brain CT is performed routinely in patients with head trauma. However, CT is not sensitive enough for subtle diffuse axial lesions, some patients with CT scans will have relatively normal results while clinically the patient has severe unexplained neurological deficits. CT can only detect hemorrhagic DAI lesions. Sensitivity depends on whether the lesions are heavily hemorrhagic. Hemorrhagic lesions can range from a few millimeters to several centimeters in diameter and are located in the white matter at the border between the white and gray matter, and in the corpus callosum and brain stem. Non-hemorrhagic lesions are areas of hypodense, which may become more apparent during the first few days as edema develops around. CT is particularly insensitive for non-hemorrhagic DAI lesions (no attenuation on CT), which can detect only 19% of such lesions, compared with 92% using magnetic resonance imaging. When the lesions are hemorrhagic and especially when the lesions are large, CT is quite sensitive. Thus often if several small hemorrhagic lesions are visible on CT, the extent of DAI is much larger.
In general, cranial CT has a low value in evaluating diffuse axonal injury.
Cranial MRI: MRI is the modality of choice for the evaluation of suspected cases of DAI, even in patients with a completely normal brain CT. MRI with SWI or GRE sequence, is highly sensitive for microhemorrhagic lesions. Some lesions may be completely non-hemorrhagic (even using SWI pulses with high magnetic fields). However, these regions will show up as regions of high FLAIR signal. It is important to note that even with modern high-field magnetic resonance machines, failure to detect does not rule out the presence of axonal damage.
MRI spectroscopy: can show increased Choline peak and decreased NAA
Recent studies also show that magnetic resonance imaging of nerve fibers (tractography) or diffusion magnetic resonance imaging (DTI - Diffusion Tensor Imaging) is valuable in detecting white matter lesions in patients with diffuse axonal lesions.
In terms of imaging, it is necessary to differentiate DAI from other diseases such as: cerebral contusion, diffuse vascular lesions, diseases that manifest with low-black signal lesions on T2* pulses such as Cerebral angiomas, chronic hypertensive encephalopathy, type IV cavernous angiomas.
In summary, DAI is a serious disease of traumatic brain injury, diagnosis of DAI is a clinical diagnosis, CT has low value in diagnosing DAI and MRI is the diagnostic modality of choice in clinical cases. ready to doubt.
The device directly affects the MRI results, so you should go to a reputable medical facility to make the diagnosis of diffuse axonal injury. Vinmec International General Hospital put into use the 3.0 Tesla Silent technology magnetic resonance imaging machine. Magnetic resonance imaging machine 3.0 Tesla with Silent technology of GE Healthcare (USA).
Silent technology is especially beneficial for patients who are children, the elderly, weak health patients and patients undergoing surgery. Limiting noise, creating comfort and reducing stress for customers during the shooting process, helping to capture better quality images and shorten the shooting time. Magnetic resonance imaging technology is the technology applied in the most popular and safest imaging method today because of its accuracy, non-invasiveness and non-X-ray use.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
References: radiopaedia.org, ncbi.nlm.nih.gov