This is an automatically translated article.
Abbreviation
Irritable Bowel Syndrome (IBS)
FODMAP: F ermentable O ligosaccharides, Disaccharides, Monosaccharides A nd P olyols
Posted by Master, Doctor Mai Vien Phuong - Department of Examination & Internal Medicine - Vinmec Central Park International General Hospital
1. Irritable Bowel Syndrome Overview
Irritable bowel syndrome (IBS) is a functional gastrointestinal (gastrointestinal) disorder that can severely impact quality of life due to abdominal pain, bloating, diarrhea, and/or constipation. The pathophysiology is complex and multifactorial, including visceral hypersensitivity, alterations in the gastrointestinal microbiota, and psychosocial factors including the gut-brain axis.
Usually, IBS is not diagnosed until other causes of symptoms have been ruled out, such as cancer, infectious colitis, inflammatory bowel disease, or celiac disease. Because the pathophysiology of IBS is multifactorial, a variety of treatments are commonly used, including management of symptoms with medication, stress management including biofeedback, and dietary interventions. This article focuses specifically on following a low-FODMAP diet (fermentable oligosaccharides, disaccharides, monosaccharides, and polyols), which has been shown to reduce symptoms in people with IBS and is included in the guidelines. National Institutes of Clinical Guidelines for Health and Care for Patients with IBS.
2. Classification of Irritable Bowel Syndrome
IBS is divided into four categories: IBS-D (IBS with diarrhea), IBS-C (IBS with constipation), IBS-M (IBS with mixed symptoms) and IBS-U (IBS unclassified) . The Rome IV criteria are used to determine the type of IBS based on abdominal pain and stool consistency; This classification is then used to guide treatment. The Gastrointestinal Symptom Rating Scale (GSRS) is a symptom assessment tool that measures the severity and baseline frequency of these symptoms, as well as response to treatment. It has been validated for both clinical and research applications in IBS patients. Many trials evaluating dietary interventions for IBS, such as the low-FODMAP diet, use GSRS to assess symptom change.
3. The introduction of a dietary intervention
The low-FODMAP diet was "born" in Australia in 2010 when a team of researchers at Monash University found that limiting foods high in FODMAPs could help reduce common IBS symptoms abdominal pain, flatulence, flatulence, diarrhea and constipation.
FODMAPs (fermentable oligosaccharides, disaccharides, monosaccharides, and polyols) are short-chain carbohydrates that are poorly absorbed from the gastrointestinal (GI) tract in some people and cause gas, bloating, and pain.
Unfortunately, many clinicians are unaware of the potential benefits of this dietary intervention or are more comfortable with the traditional pharmacological approach to IBS treatment.
"Raising awareness of the low-FODMAP diet among both clinicians and patients is important because the two approaches are synergistic and not mutually exclusive".
4. The Science Behind the FODMAP Diet
The science behind this dietary approach is strong and includes many randomized controlled trials comparing the low FODMAP diet with many other interventions in patients with IBS,
"The Bottom Line is that when you look at the data through a meta-analysis, such as ours, they show that the low-FODMAP diet offers a greater benefit than these comparisons." William D. Chey, MD, Professor of Digestive Science & Nutrition at the University of Michigan Health System in Ann Arbor
. "The only randomized controlled trial from the United States was published by our team and has shown that the biggest benefits [of the diet] are pain and bloating."
5. Effect of FODMAP
"Up to 70%-80% of patients with IBS may benefit, to some extent, from a low-FODMAP diet," says Eamonn M. Quigley, MD, director of the Lynda King Center. and David M. Underwood said Gastrointestinal Disorders at Houston Methodist Hospital. However, he notes that "it's difficult to do because it excludes many nutrient-rich foods, as well as foods that act as substrates for beneficial gut bacteria."
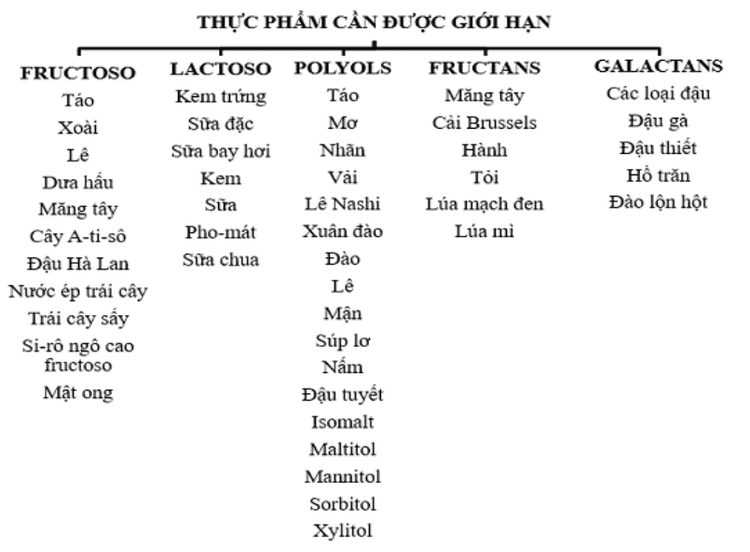
Examples of foods that are not allowed on the low-FODMAP diet include wheat, rye, onions, legumes and garlic, which are rich in oligosaccharides; dairy products rich in lactose (a commonly known disaccharide); and high-fructose fruits, as well as fruits, vegetables, and artificial sweeteners high in mannitol and sorbitol.
Treatment goals are often designed to align with outcome measures used in these studies, such as GSRS. This is important for standardizing the diet to determine which foods are most likely to trigger symptoms. In addition, each patient should define his or her own goals for therapy. For example, one patient may focus most on reducing the frequency or urgency of diarrhea, while another may prioritize reducing abdominal pain and bloating. Often, treating one symptom helps alleviate others, but patients need to focus on a “what works for them” framework in order to remain fully motivated and adhere to a restrictive diet. so.
6. Dietary Interventions for IBS Patients - The Low FODMAP Diet
In a recent survey of 1,562 gastroenterologists in the United States, nearly 60% indicated that at least half of patients with IBS associated food with their digestive symptoms. Before seeking treatment with a gastroenterologist, patients are more likely to use a 'trial and error', or lactose-free or gluten-free diet than to try a low-FODMAP diet.13Read More half of gastroenterologists recommend dietary therapy 75% of their patients have IBS with the low FODMAP diet being the most common.
For many people, foods containing FODMAPs (all carbohydrates), have been shown to worsen IBS.14-16 Consuming a diet that restricts foods high in FODMAPs has been shown It has been shown to reduce symptoms and thus improve quality of life in 50-80% of IBS patients. FODMAPs are highly permeable (absorb water into the intestine), poorly absorbed, and are rapidly fermented by intestinal bacteria leading to excess gas production.
FODMAP-rich foods are classified into those containing fructans/galacto-oligosaccharides (GOS), lactose, excess fructose (fructose to glucose ratio > 1), and polyols. Some foods may contain more than one type. Table 2 provides resources to help identify the foods in each category.
Fructan and Galacto-oligosaccharides (GOS)
Fructan are fructose polymers (oligosaccharides) found in many foods, including onions, garlic, and some fruits and grains. Also included in this category are inulin and fructo-oligosaccharides that are added to many foods as prebiotics. The small intestine (small intestine) cannot hydrolyze the fructose-fructose bonds, so fructan enters the large intestine instead of being absorbed in the small intestine. In the colon, they are fermented by colonic bacteria, causing symptoms associated with IBS in people with visceral hypersensitivity. Wheat, onions, and garlic are very common fructans in the U.S. food supply. GOS molecules composed of galactose-galactose bonds also cannot be hydrolyzed or absorbed in the small intestine, causing symptoms similar to fructans in the colon. Lentils, chickpeas (and thus peas), and red beans are common sources of GOS.
Lactose sugar
Many individuals, even those without IBS, are lactose intolerant or allergic to lactose. Lactose is a disaccharide of glucose and galactose, which is normally hydrolysed in the brush border of the proximal small intestine. When lactose is not absorbed, disaccharides can create gas and tension in both the small intestine and colon. Common sources of lactose include milk, ice cream/cream, yogurt, and some cheeses.
Fructose
Fructose is more easily absorbed in SBP in the presence of glucose, so foods with excess fructose relative to glucose will lead to fructose malabsorption. People with IBS and visceral hypersensitivity will experience bloating, pain, and bloating due to this fructose malabsorption response. Foods with excess fructose include, but are not limited to, watermelon, pineapple, honey, apples, pears, and all foods and beverages with high fructose corn syrup.

Polyols
Polyols are reduced calorie/carbohydrate sweeteners, commonly known as sugar alcohols (such as sorbitol, mannitol, xylitol, isomalt). Sorbitol and mannitol occur naturally in foods like mushrooms, avocados, prunes/prune juice, and iced fruit, but are also added to sugar-free foods like gelatin, puddings, and beverages.
Xylitol and isomalt are added to commercial sweeteners such as chewing gum and products marketed as “sugar free”. These polyols are absorbed slowly along the length of the small intestine. They normally reach the colon, where they act as osmotic agents that pull fluid into the intestines and are fermented by colonic bacteria. This causes the 'flatulence and tension' common in IBS. All individuals, not just those with IBS, are prone to diarrhea when consuming these products in large amounts, hence the warning on many products containing artificially added sugar alcohols - "consume in excess may have a laxative effect." People with IBS may have a lower response threshold to polyols.
7. Implement the FODMAP diet based on the doctor-patient relationship
Although following a low FODMAP diet can be challenging, a survey of gastroenterologists found that only 21% of gastroenterologists routinely refer IBS patients to a specialist. nutritionist (Nutritionist), demonstrating the need to improve interdisciplinary care for these patients. Dietitians should complete a nutrition assessment and develop a nutritional care plan to help patients and others plan a successful low-FODMAP diet.
The dietician should first conduct anthropometry and dietary history. Some patients with IBS may self-identify as overweight or unsatisfied due to frequent bloating when eating. Dietitians should work with patients to establish healthy and reasonable weight goals, if needed. The food frequency questionnaire can be a useful dietary history tool, as this will highlight foods or food groups that have been avoided due to symptom induction, intolerance. or known allergies. It is important to note that foods that are consumed regularly are high in FODMAPS, suggesting food alternatives to these foods.
Conclusion
The FODMAP diet has been improved to improve IBS symptoms. With careful planning, this diet can be nutritionally complete. Significantly improving quality of life for people with IBS can promote dietary adherence. Gastroenterologists should refer IBS patients to a Dietitian for nutritional assessment, education, and dietary planning.
Currently, Vinmec International General Hospital is a prestigious address trusted by many patients in performing diagnostic techniques for digestive diseases, diseases that cause chronic diarrhea, Crohn's disease, gastric mucosa Esophageal ectopic... Along with that, at Vinmec Hospital, screening for gastric cancer and gastric polyps is done through gastroscopy with an Olympus CV 190 endoscope, with NBI (Narrow) function. Banding Imaging - endoscopy with narrow light frequency) results in clearer images of mucosal pathology than conventional endoscopy, detecting ulcerative colitis lesions, digestive cancer lesions Early stage...
Vinmec Hospital with modern facilities and equipment and a team of experienced specialists who are always dedicated in medical examination and treatment, customers can rest assured with internal services. gastroscopy, esophagoscopy at Vinmec International General Hospital.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
References
Definition and Facts for Irritable Bowel Syndrome. National Institute of Diabetes and Digestive and Kidney Diseases website. National Institutes for Health, U.S. Department of Health and Human Services. https://www.niddk.nih.gov/ health-information/digestive-diseases/irritable-bowel-syndrome/definition-facts. Updated November 2017. Accessed February 21, 2018. Irritable syndrome in bowel adults: diagnosis and management of irritable bowel syndrome in primary care. Clinical Guideline 61. National Institute for Health and Clinical Excellence website. Available at: https://www.nice.org.uk/ guidance/cg61. Updated April 2017. Accessed February 22, 2018. Kanazawa M, Hongo M, Fukudo S. Visceral hypersensitivity in irritable bowel syndrome. J Gastro Hep. 2011;26(suppl 3):119-121. Carol Rees Parrish, M.S., R.D., Series Editor, When a Registered Dietitian Becomes the Patient: Practical gastroenterology • may 2018