This is an automatically translated article.
Posted by Master, Doctor Mai Vien Phuong - Department of Examination & Internal Medicine - Vinmec Central Park International General Hospital
Abbreviation
Irritable Bowel Syndrome (IBS)
FODMAP: F ermentable O ligosaccharides, Disaccharides, Monosaccharides A nd P olyols
Irritable bowel syndrome (IBS) can seriously affect quality of life due to abdominal pain, bloating, diarrhea and/or constipation. Symptoms can be improved by following a diet low in fermentable oligosaccharides, disaccharides, monosaccharides, and polyols (FODMAP), but implementing this restrictive diet can be challenging. This article provides guidance for all 3 phases of the low-FODMAP diet for the treatment of irritable bowel syndrome.
1. Irritable Bowel Syndrome Overview
Irritable bowel syndrome (IBS) is a functional gastrointestinal (gastrointestinal) disorder that can severely impact quality of life due to abdominal pain, bloating, diarrhea, and/or constipation. The pathophysiology is complex and multifactorial, including visceral hypersensitivity, alterations in the gastrointestinal microbiota, and psychosocial factors including the gut-brain axis. Often, IBS is not diagnosed until other causes of symptoms have been ruled out, such as cancer, infectious colitis, inflammatory bowel disease, or celiac disease.
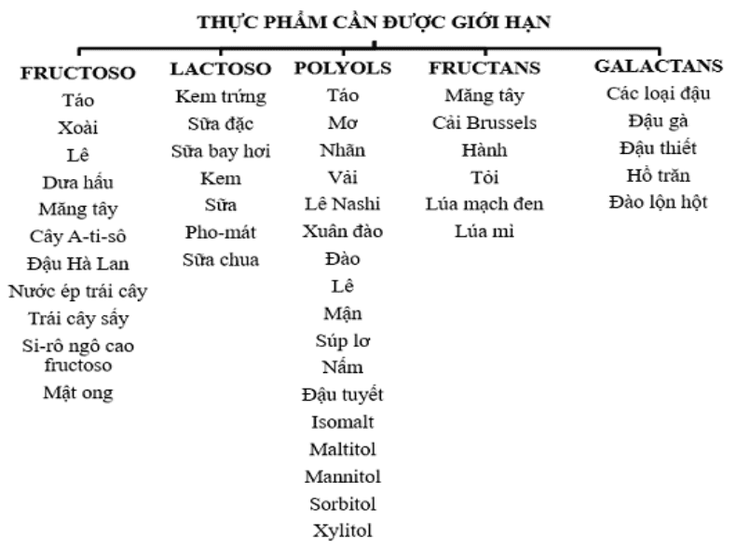
Because the pathophysiology of IBS is multifactorial, a variety of treatments are commonly used, including medication management of symptoms, stress management including biofeedback, and dietary interventions . This article focuses specifically on following a low-FODMAP diet (fermentable oligosaccharides, disaccharides, monosaccharides, and polyols), which has been shown to reduce symptoms in people with IBS and is included in the guidelines. National Institutes of Clinical Guidelines for Health and Care for Patients with IBS.
2. Classification of irritable bowel syndrome
IBS is divided into four categories: IBS-D (IBS with diarrhea), IBS-C (IBS with constipation), IBS-M (IBS with mixed symptoms) and IBS-U (IBS unclassified) . The Rome IV criteria are used to determine the type of IBS based on abdominal pain and stool consistency; This classification is then used to guide treatment.
The gastrointestinal symptom rating scale (GSRS) is a symptom assessment tool that measures the severity and baseline frequency of these symptoms, as well as response to treatment. It has been validated for both clinical and research applications in IBS patients. Many trials evaluating dietary interventions for IBS, such as the low-FODMAP diet, use GSRS to assess symptom change.
3. Importance of a holistic approach to treatment - expert opinion
In the management of patients with IBS, and also IBD, experts believe that clinicians should use all the tools available to them. This includes combining integrative medicine with standard pharmacology.
Author Chey says: "It is becoming increasingly clear that a more holistic, holistic approach is needed in the care of these patients." "Such an approach, which may incorporate diet, behavioral techniques such as cognitive-behavioral therapy or hypnosis, and medications, should be tailored based on the patient's symptoms and We often use a multimodal approach in IBS patients that combines medication with dietary and behavioral interventions.”
As far as the low-FODMAP diet, Chey says one study recently performed by his team showed that it led to significant improvements in both quality of life and anxiety compared with conventional dietary recommendations. found that as digestive symptoms get better, quality of life and anxiety get better."
In fact, the University of Michigan, where Chey practices, runs one of the specialist programs first digestible nutrition in the United States in 2008, and it continues to be a hub for clinicians and patients interested in learning more about the benefits of Dietary interventions for digestive conditions.
King recommends clinicians and patients visit FODMAPs every day and use resources compiled by IBS expert Kate Scarlata, RDN, as well as connect with a local dietitian through the site. Web site of the Institute of Nutrition and Dietetics.
King also notes: "Resolving IBS symptoms early in the course of disease with a low-FODMAP diet can save patients from resorting to more aggressive pharmacological therapy and continuing associated discomfort. to this state."
4. A Personal Diet Protocol, Not Just a Diet
Author Chey explains that the low-FODMAP diet is actually a three-phase diet consisting of a 2- to 4-week FODMAP elimination phase, followed by a gradual reintroduction of FODMAP-containing foods. individually to determine patient sensitivities and then liberalize the diet in the terminal phase.
"Usually, patients who will respond get better in a 2-week period, but sometimes it can take up to 4 weeks for some people to see a benefit," he says. "Patients who do not respond within the 2 to 4 week time frame should be switched to some other form of therapy. Among those who respond, approximately 85% or more can liberalize the diet in long periods and make them less restrictive."

5. FODMAP diet in pediatric patients
King says the situation in pediatric patients is similar. "In our clinical experience, we find that within 2 weeks, patients either improve or they don't. If there's no improvement within 6 weeks, I recommend talking to a provider. health care services and a return to a regular diet."
According to Chey, a low-FODMAP diet may also be beneficial for other digestive conditions, including inflammatory bowel disease (IBD).
"We are increasingly using this diet in patients who have IBD and are in remission of their inflammation but still have symptoms, like abdominal pain and changes in bowel habits," he says. "Again, symptoms likely to respond to this diet are pain and bloating. Some patients will also experience diarrhea-related benefits, but we found that this did not. consistent or reliable
6. What's important in the FODMAP diet?
Treatment goals are often designed to match the outcome measures used in these studies, such as gastrointestinal symptom assessment. This is important for standardizing the diet to determine which foods are most likely to trigger symptoms. In addition, each patient should define his or her own goals for therapy. For example, one patient may focus most on reducing the frequency or urgency of diarrhea, while another may prioritize reducing abdominal pain and bloating. Often, treating one symptom helps alleviate others, but patients need to focus on a “what works for them” framework in order to remain fully motivated and adhere to a restrictive diet. so.
Currently, Vinmec International General Hospital is a prestigious address trusted by many patients in performing diagnostic techniques for digestive diseases, diseases that cause chronic diarrhea, Crohn's disease, gastric mucosa Esophageal ectopic... Along with that, at Vinmec Hospital, screening for gastric cancer and gastric polyps is done through gastroscopy with an Olympus CV 190 endoscope, with NBI (Narrow) function. Banding Imaging - endoscopy with narrow light frequency) results in clearer images of mucosal pathology than conventional endoscopy, detecting ulcerative colitis lesions, digestive cancer lesions Early stage...
Vinmec Hospital with modern facilities and equipment and a team of experienced specialists who are always dedicated in medical examination and treatment, customers can rest assured with internal services. gastroscopy, esophagoscopy at Vinmec International General Hospital.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
References
Definition and Facts for Irritable Bowel Syndrome. National Institute of Diabetes and Digestive and Kidney Diseases website. National Institutes for Health, U.S. Department of Health and Human Services. https://www.niddk.nih.gov/ health-information/digestive-diseases/irritable-bowel-syndrome/definition-facts. Updated November 2017. Accessed February 21, 2018. Kanazawa M, Hongo M, Fukudo S. Visceral hypersensitivity in irritable bowel syndrome. J Gastro Hep. 2011;26(suppl 3):119-121. Carol Rees Parrish, M.S., R.D., Series Editor, When a Registered Dietitian Becomes the Patient: Practical gastroenterology • may 2018














