This is an automatically translated article.
The article was written by Dr. Nguyen Khanh Hoa - Research project manager, VinmecResearch Institute of Stem Cells and Gene Technology
Nonalcoholic steatohepatitis (NASH) is becoming one of the leading causes of hepatocellular carcinoma (HCC). Sorafenib is the only first-line therapy for advanced HCC despite its serious side effects.
1. What is Sorafenib?
Sorafenib is currently the only US FDA-approved first-line therapy for advanced hepatocellular carcinoma (HCC). It is a potent inhibitor of many kinases, especially the raf signaling chain including (ERK) kinase (MEK), which acts on anti-tumor mechanisms by inhibiting proliferation, inducing apoptosis and prevent angiogenesis.
As a multi-kinase inhibitor, sorafenib has been reported to affect many important processes in HCC and injury. Our data made it clear that independent of its major kinase targets, activation of AMPK signaling is important for the function of sorafenib in NASH.
However, the therapeutic efficacy of sorafenib in the treatment of HCC is not satisfactory. An oral treatment of sorafenib at 400 mg twice daily only extended the overall median survival by 2.8 months.
Furthermore, at this dose, sorafenib causes serious and widespread side effects including fatigue, loss of appetite, diarrhea, rash and peeling, skin reactions of the limbs, and increased blood pressure. These side effects significantly limit the tolerability of the drug in the clinical setting of its beneficial effects.
2. Benefits of sorafenib in NASH
Mechanistically, the benefit of sorafenib in NASH is independent of its active kinase targets in HCC, but is related to the induction of mild mitochondrial uncoupling and subsequent activation of protein kinases for activation. AMP (AMPK) chemistry.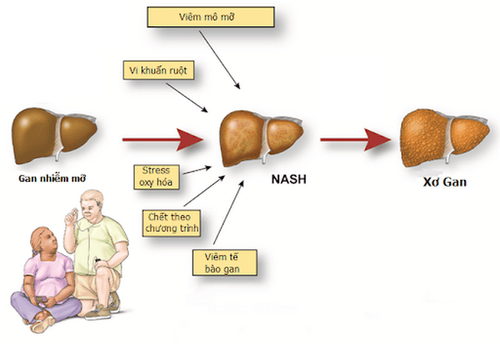
NASH - Viêm gan nhiễm mỡ không do rượu
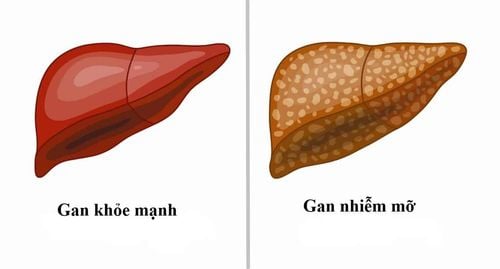
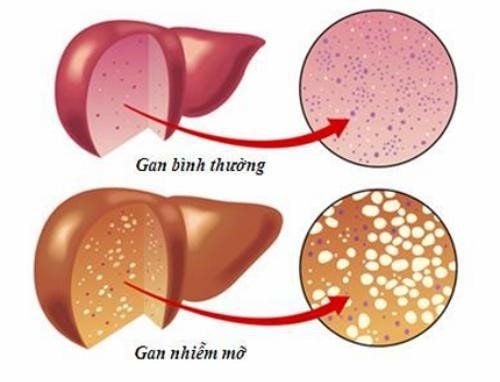
3. Situation of non-alcoholic steatohepatitis
The prevalence of non-alcoholic steatohepatitis (NASH) is increasing sharply and becoming a leading cause of end-stage liver disease, including cirrhosis, hepatocellular carcinoma (HCC) and liver failure. Sorafenib remains the current first-line and sole treatment for HCC despite serious side effects at clinical doses.
In this study, Jian et al. reported that treatment with sorafenib in both rat and monkey models of NASH was equivalent to one in ten clinical outcomes. The dose addressed key signs of disease, including fatty liver, inflammation, and fibrosis, without detectable toxicity. These data suggest a potential clinical application of low-dose sorafenib as a NASH therapy with less risk of adverse events currently observed with its use in the treatment of HCC.
The benefits of AMPK activation for NASH therapy may be achieved by the regulation of fatty acid metabolism homeostasis, which contributes to the reduction of inflammation. AMPK activation also directly phosphorylates caspase-6 to inhibit lipotoxicity-induced hepatocellular death in NASH. Furthermore, addressing fibrosis through the AMPK-mTOR pathway could also be a therapeutic effect of AMPK in liver fibrosis.

Bệnh viêm gan nhiễm mỡ không do rượu cần được điều trị sớm
However, the benefit of mTOR inhibitors for liver injury is controversial. The observation that sorafenib inhibits mTOR activity is consistent with previous reports that mTOR inhibition can revert the metabolic dysregulation. However, attempting to inhibit mTORC1 by removing the liver-specific Raptor worsens liver injury and tumorigenesis. This paradox indicates that the balance of mTOR activity is important for liver pathogenesis.
Inferring the appropriate timing and dosage of sorafenib to sufficiently inhibit mTOR and/or downstream mTOR-independent signals that activate AMPK may explain the beneficial effects of sorafenib in NASH.
According to research, this is the first time sorafenib has demonstrated mitochondrial-independent effects, although impaired mitochondrial function has been linked to its cancer-killing ability.
Data suggest that, under nutritional overload conditions, mild mitochondrial cleavage induced by low-dose sorafenib burns excess nutrients, activates AMPK, and protects against metabolic disease, notably I mean NASH. Mitochondrial independence, defined as a useless stream of protons that does not produce ATP, has long been considered a therapeutic target for metabolic diseases. For example, the 2,4-dinitrophenol (DNP) mitochondrial splitter was approved for obesity in the 1930s, but was withdrawn from the market due to the risk of fatal hyperthermia.
Recently, the Gerald Shulman group developed several targeted liver derivatives of DNP, mitochondrial-independent energy production and safely reversing fatty liver, hepatitis, and cirrhosis in rodents. and the primate model is not yours.
Furthermore, some chemicals, such as salicylate and niclosamide ethanolamine, have been shown to improve fatty liver and diabetes by inducing mitochondrial detachment.

Hoá chất niclosamide ethanolamine có thể cải thiện tình trạng gan nhiễm mỡ
Customers can directly go to Vinmec Health system nationwide to visit or contact the hotline here for support.