This is an automatically translated article.
Posted by Doctor Mai Vien Phuong - Department of Medical Examination & Internal Medicine - Vinmec Central Park International General Hospital.Patient has prolonged hoarseness, went to many places, met many otolaryngologists, but still no relief. It was time to see a gastroenterologist, found that the patient had reflux esophagitis, and the doctor concluded that the patient's hoarseness was caused by reflux esophagitis. What are the characteristics of this disease? Why can reflux esophagitis cause persistent hoarseness? This article will address that issue.
1. Overview of Reflux esophagitis (also known as Gastroesophageal Reflux)
Gastroesophageal reflux disease (GERD) is a common gastrointestinal (GI) disease with worldwide prevalence and high prevalence in Western countries. The 2006 Montreal Consensus defined gastroesophageal reflux disease as a condition that develops when the reflux of gastric contents causes troublesome symptoms and/or complications into the esophagus. Tissue damage associated with gastroesophageal reflux disease ranges from esophagitis to Barrett's esophagus and adenocarcinoma of the esophagus; The troubling symptoms of reflux can be esophageal (regurgitation, regurgitation) or extraesophageal. Gastroesophageal reflux disease can be further classified by the presence of an erosive stain on endoscopic examination (Erosive Reflux Disease [ERD] and Non-Erosive Reflux Disease [NERD]).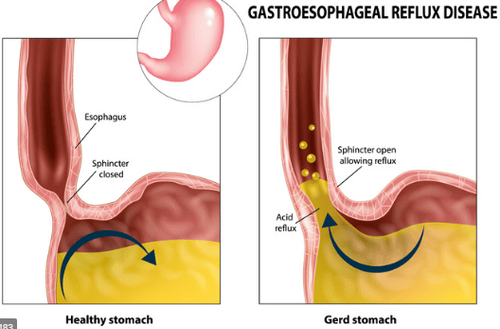
Extraesophageal manifestations associated with gastroesophageal reflux disease are frequent and represent a diagnostic and therapeutic challenge, possibly involving the lungs, upper respiratory tract, and mouth, presenting with asthma, laryngitis, chronic cough, tooth wear and non-cardiac chest pain
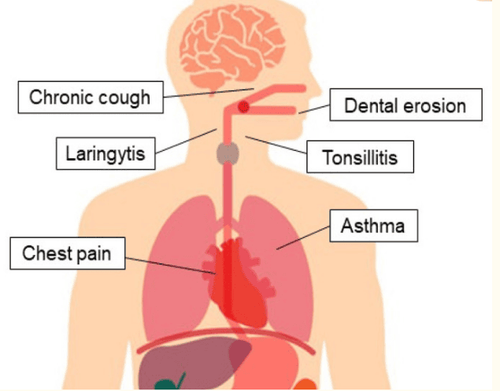
2. Laryngitis. management and pharynx. This is a common extraesophageal presentation associated with gastroesophageal reflux disease: up to 10–15% of all visits to ENT clinics are due to manifestations of laryngeal reflux- oropharyngeal
Laryngeal symptoms of gastroesophageal reflux disease
Gastroesophageal reflux disease can cause many laryngeal symptoms, such as hoarseness, sore or burning throat, pain when swallowing, feeling of a lump in the throat, cough, repetitive clearing of the throat, a lot of phlegm, difficulty swallowing, and voice fatigue. These complaints are not specific to gastroesophageal reflux disease and laryngopharyngeal reflux disease, and they may also be caused by allergens, smoke, and various irritants. In a large case-control study, patients with esophagitis or esophageal stricture had a higher odds ratio (OR) for pharyngitis (OR: 1.60), anorexia (OR: 1.81) and chronic laryngitis (OR: 2.01) compared with the control group. Many patients diagnosed with GERD do not suffer from the classic symptoms of gastroesophageal reflux disease: heartburn is absent in more than half of patients with laryngopharyngeal reflux. In the gastroesophageal reflux disease PRO study, the incidence of laryngeal dysfunction was 10.4%, and it was associated with older age, longer duration of GERD, and obesity. Interestingly, smokers are less likely to have laryngeal disorders than non-smokers, possibly because the laryngeal mucosa is desensitized.
Why does gastroesophageal reflux disease cause this problem in the larynx
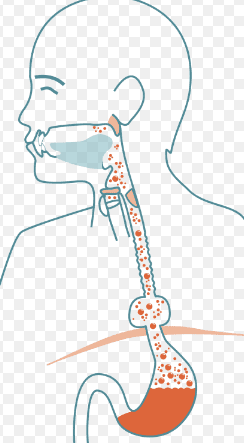
The laryngeal manifestation of gastroesophageal reflux disease can be explained by direct damage caused by acid exposure- peptides in the larynx via esophago-oropharyngeal reflux (micro-aspiration theory), or by indirect acidification of the distal esophagus via an intermediate reflex (esophagobronchial reflex theory). Both mechanisms lead to chronic clearing of the throat and cough, causing mucosal damage and typical signs and symptoms.
Laryngeal mucosa is more susceptible to damage than esophageal mucosa: acid reflux, containing acid and pepsin, and bile reflux cause inflammatory lesions and precancerous lesions of the larynx. However, the inability to clear saliva leads to more severe damage than that of the esophagus.
3. How to diagnose? Laryngoscopy revealed reflux-mediated disease as erythema, edema, lymphatic hyperplasia of the posterior larynx wall, ulceration, stenosis of the lower glottis or posterior glottis, vocal cord polyps, granulomas, and leukocytes. cancer. Although common in reflux laryngitis, most of them are nonspecific. Edema and congestion, commonly used to define reflux laryngitis, lack specificity and are highly operator-dependent parameters: in fact, signs of laryngeal irritation are present in more than 80% of healthy controls. Allergies, smoking, and voice abuse are common causes of laryngeal irritation and cause similar alterations of laryngopharyngeal reflux.
Role of esophageal pH monitoring
The use of ambulatory esophageal pH monitoring to diagnose laryngopharyngeal reflux is controversial. Monitoring pH of the proximal esophagus and pharynx has a sensitivity of 40% and 55%, respectively. Although pH monitoring detects reflux only in 40% of patients with symptoms of laryngeal dysfunction, impedance monitoring can detect the presence of weak acid and alkali, gas, and acid reflux. or fluid that can cause laryngeal dysfunction.
Test for the detection of pepsin in saliva
A promising noninvasive test for the diagnosis of reflux, although still controversial in its clinical applications, is the detection of pepsin in saliva. Pepsin is a proteolytic enzyme secreted in the gastric lumen as pepsinogen and activated in an acidic environment: its determination at non-gastric sites can detect the presence of significant reflux. . Methods for measuring pepsin concentrations have not yet been standardized, with inconsistent accuracy. Using Western blot technique to sample sputum and salivary pepsin in patients with GERD, Kim et al. reported a sensitivity and specificity of 89% and 68%, respectively, based on pH monitoring results. . Monoclonal antibody testing has shown recent, prospective, blinded positive and negative predictive values of 87% and 78%, respectively.
4. Treatment
Hanson et al. reported a high response rate for medical and non-medical laryngopharyngeal reflux: half of the patients responded to behavioral changes, while 54% of those were unsuccessful. with this method reacts with H2 blockers. PPI therapy is the standard treatment in patients with chronic pharyngeal symptoms if GERD is suspected to be the underlying cause, although single-dose PPI therapy has not been shown to be effective. superiority over placebo in the treatment of laryngopharyngeal reflux. An experimental trial of a double dose PPI recommended as first-line therapy in patients with suspected laryngopharyngeal reflux for positive suppression of oropharyngeal acid reflux. A 2016 meta-analysis of 13 RCTs in patients with laryngopharyngeal reflux showed improvement in reflux symptoms (as measured by the reflux symptom index [RSI]) with twice-daily treatment. days for 3–6 months, although there was no observed difference in response rates and effects on the laryngeal mucosa between PPIs and placebo. On the other hand, a recent meta-analysis of controlled studies including patients with laryngopharyngeal reflux showed no benefit from PPI therapy. This negative finding could be partly explained by the difficulty in identifying patients with laryngopharyngeal reflux, since there are no specific diagnostic tools. The diagnosis of gastroesophageal reflux disease-associated laryngitis is presumed to be the presence of symptoms such as throat clearing, cough, and lymphadenopathy, and signs such as laryngeal edema and erythema, although these are Symptoms are not specific for reflux. Patients who do not respond to PPI therapy may have disease related to nonreflux or a functional component. The lack of efficacy of PPIs in clinical trials can also be explained by the high placebo response rate, approximately 40%.
Recommended initial treatment approach
Empiric PPI therapy for a period of one or two months is a reasonable initial approach in patients with no warning symptoms and a high suspicion of associated laryngeal disease. regarding reflux. If symptoms improve, therapy can be continued for up to 6 months to allow healing of laryngeal tissue, after which the dose should be tapered to minimal acid suppression, resulting in a sustained response. In patients who do not respond to PPIs, impedance or pH monitoring may be used to rule out reflux as the cause of laryngeal complaints.
Combination of PPIs and prokinetics is recommended.
Ren et al evaluated the combination of PPIs and prokinetics as effective in improving QoL, although it did not have a significant effect on symptoms or reactions. Endoscopic effects of extraoesophagitis associated with gastroesophageal reflux disease.
Role of dietary changes
Among the non-pharmacological treatments for laryngopharyngeal reflux, dietary changes have been shown to be effective: patients follow a low-fat diet , more protein and alkaline have a higher rate of symptom resolution. However, a recent systematic review concluded that there is insufficient evidence to recommend dietary modification for laryngopharyngeal reflux.
Conclusion
The diagnosis of extraesophageal manifestations associated with gastroesophageal reflux disease is not simple and is often excluded. Esophagogastroduodenoscopy plays a secondary role, more useful if alarming symptoms are present. 24-hour esophageal pH monitoring is relevant in the diagnosis of extraesophageal manifestations. This test allows the diagnosis of acid reflux events in the esophagus and, using pH impedance monitoring, the reflux of both acidic and non-acidic materials into the esophagus can also be identified. The PPI test is often used as the first diagnostic step. In atypical cases, diagnostic tools such as laryngoscopy and bronchoscopy may be useful to detect abnormalities associated with reflux lesions.
Currently, Vinmec International General Hospital is a prestigious address trusted by many patients in performing diagnostic techniques for digestive diseases, diseases that cause chronic diarrhea, Crohn's disease, gastroesophageal reflux disease. Along with that, at Vinmec Hospital, screening for stomach cancer and gastric polyps is done through gastroscopy with Olympus CV 190 endoscope, with NBI (Narrow Banding Imaging - endoscopy with narrow light frequency band) results in clearer images of mucosal pathology than conventional endoscopy, detecting ulcerative colitis lesions, early gastrointestinal cancer lesions ...
Vinmec Hospital with modern facilities and equipment and a team of experienced experts who are always dedicated in medical examination and treatment, customers can rest assured with gastroscopy service. , esophagus at Vinmec International General Hospital.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
References 1. Marilena Durazzo,1,2,* Giulia Lupi, Extra-Esophageal Presentation of Gastroesophageal Reflux Disease: 2020 Update, J Clin Med. 2020 Aug; 9(8): 2559.Vakil N., Van Zanten S.V., Kahrilas P., Dent J., Jones R., Global Consensus Group The Montreal definition and classification of gastroesophageal reflux disease: A global evidence-based consensus. Am. J. Gastroenterol. 2006;101:1900-1920. doi: 10.1111/j.1572-0241.2006.00630.x. [PubMed] [CrossRef] [Google Scholar] Kahrilas P.J., Altman K.W., Chang A.B., Field S.K., Harding S.M., Lane A.P., Lim K., McGarvey L., Smith J., Irwin R.S., et al. Chronic cough due to gastroesophageal reflux in adults: CHEST guideline and expert panel report. Chest. 2016;150:1341–1360. doi: 10.1016/j.chest.2016.08.1458. [PMC free article] [PubMed] [CrossRef] [Google Scholar]














