This is an automatically translated article.
Posted by Doctor Mai Vien Phuong - Department of Medical Examination & Internal Medicine - Vinmec Central Park International General Hospital.
Laryngeal reflux is defined as the reflux of gastric contents into the larynx and pharynx. A large amount of data suggest an increasing prevalence of laryngeal symptoms in patients with gastroesophageal reflux disease.
1. Introduction
Laryngeal reflux (LPR) is defined as the reflux of stomach contents into the larynx and pharynx. According to the Montreal Consensus, manifestations of gastroesophageal reflux disease (GERD) have been classified as esophageal or extraesophageal syndromes and among the following, the existence of an association between laryngeal reflux and gastroesophageal reflux disease have been established.
Laryngeal reflux can be manifested by laryngeal symptoms such as cough, sore throat, hoarseness, difficulty in breathing and swallowing, as well as signs of laryngeal irritation on laryngoscopy. Laryngeal symptoms are increasingly recognized by general practitioners, pulmonologists, and ENT surgeons. In particular, there is a large amount of data on the increasing prevalence of laryngeal symptoms in 60% of patients with GERD.
In addition, several studies support the view that gastroesophageal reflux disease, as well as smoking and alcohol use, are risk factors for colon cancer. According to the Montreal Consensus, several important issues were highlighted, as follows:
Rarity of isolated extraesophageal syndromes that do not present concomitantly with reflux disease symptoms typical gastroesophageal reflux (ie, heartburn and regurgitation); Extraesophageal syndrome is often multifactorial with gastroesophageal reflux disease being one of several potential cofactors for exacerbation; Data supporting a beneficial effect of reflux treatment for extraesophageal syndrome are weak. Subsequently, the American Gastroenterology Association guidelines for gastroesophageal reflux disease recommend against the use of acid-suppressing therapy for acute treatment of patients with gastroesophageal reflux disease syndrome. extraesophageal (laryngitis, asthma) in the absence of typical gastroesophageal reflux disease symptoms.
2. Mechanism of laryngeal reflux
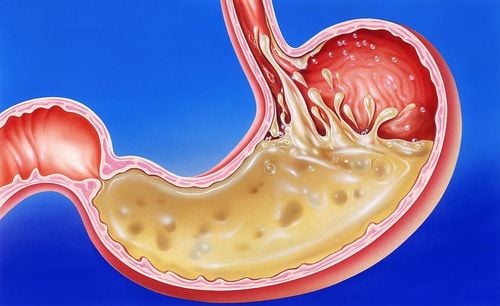
The specific mechanisms involved in reflux leading to laryngeal signs and symptoms are currently unknown. The acidity of gastric juice alone can cause tissue damage in the upper respiratory tract, but several studies have demonstrated that this is not the only etiological factor involved in the pathogenesis of laryngeal reflux disease. manage .
Indeed, Pearson et al recently emphasized that, although acidity can be controlled with proton pump inhibitor (PPI) therapy, all other harmful factors (eg, pepsin, bile salts) , bacteria, and pancreatic proteolytic enzymes) are still potentially harmful with PPI treatment and may increase their potential for harm. In particular, pepsin can damage all tissues beyond the stomach at pH up to 6. Notably, Johnston et al. have shown that detectable levels of pepsin remain in the posterior laryngeal epithelium. a reflux event. The same authors described that pepsin is absorbed by laryngeal epithelial cells by receptor-mediated endocytosis, thus it may represent a novel mechanism, besides its proliferative activity. proteolytic alone, whereby pepsin can induce gastroesophageal reflux disease-associated cell damage independent of the pH of the reflux substance.
3. Difficulty in diagnosing laryngeal reflux disease
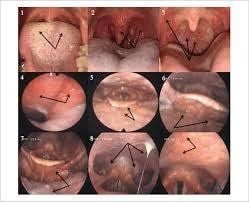
Until now, the diagnosis of laryngopharyngeal reflux is a very difficult task and there is still some controversy about how to confirm laryngeal reflux. Laryngoscopy findings, particularly edema and congestion, are commonly used to diagnose laryngeal reflux by ENT surgeons. It should be pointed out, however, that, in a well-conducted prospective study, laryngoscopy revealed one or more signs of laryngeal irritation in more than 80% of healthy controls. Furthermore, it has been shown that accurate clinical assessment of laryngeal reflux can be difficult because physical findings of the larynx cannot be reliably determined from clinician to physician. clinician, and such variability makes for an accurate laryngoscopy diagnosis of very dominant laryngeal reflux. The sensitivity and specificity of ambulatory pH monitoring as a means of diagnosing gastroesophageal reflux disease in patients with symptoms of extraesophageal reflux have been tried. Furthermore, the sensitivity of two-probe monitoring (esophagus and pharynx) for 24 h ranged from 50% to 80%.
4. The role of esophageal manometry and esophageal pH monitoring (MII-pH)
Recently, the availability of multichannel intraluminal impedance (oesophageal manometry) and esophageal pH monitoring (MII-pH) seem to be more effective in diagnosing extranodal manifestations. management of gastroesophageal reflux disease by its ability to evaluate the reflux of acid and other non-acid components in the stomach.
However, the poor sensitivity and specificity of all available diagnostic tests for laryngeal reflux have been highlighted by several review articles. In a population of patients with laryngoscopy detecting laryngeal reflux, multiple studies have shown that esophageal pH measurement confirms the diagnosis of gastroesophageal reflux disease in less than 40% of patients, thus highlighting the problem. importance of nonspecific symptoms and laryngoscopy findings of laryngeal reflux.
Promising new diagnostic techniques have been developed for extraesophageal reflux syndromes, especially the immunosorbent pepsin test (Peptest TM), which has been shown to be a rapid, sensitive and specific tool , and an oropharyngeal pH catheter (manufactured by Retech, San Diego, CA, USA) which recent research has documented as a highly sensitive and minimally invasive device for detecting fluid or Vapors of acid reflux in the back of the pharynx . However, limited data on their diagnostic accuracy and potential clinical application are available.
5. Obesity and laryngeal reflux disease
The prevalence of obesity in Western countries has increased significantly, and this has coincided with an increase in the number of patients with gastroesophageal reflux disease. Numerous epidemiological studies have clearly demonstrated an association between obesity and gastroesophageal reflux disease, and investigations support a biologically plausible relationship between obesity and gastroesophageal reflux disease. In particular, various studies have shown an association between higher body mass index (BMI) and gastroesophageal reflux disease and also obesity (BMI > 30 kg/m2) and Being overweight (BMI 25–30 kg/m2) is associated with gastroesophageal reflux disease. The effect of BMI on the occurrence of gastroesophageal reflux disease does not appear to be dependent on total calories, fiber intake, fruits and vegetables, or other macro or micronutrients.
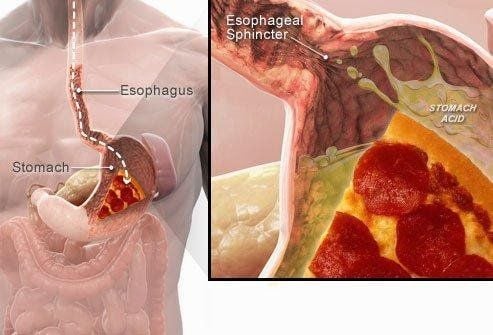
6. The role of the esophagus-stomach junction
Obesity is thought to alter the morphology and function of the gastroesophageal junction (EGJ). Indeed, obesity induces mechanical disruption of the gastroesophageal junction by promoting axial separation between the lower esophageal sphincter (lower esophageal sphincter) and the external diaphragm. Ineffectiveness of the lower esophageal sphincter has also been observed in obese patients and among obese patients with the disease, higher esophageal acid exposure is significantly associated with muscle pressure. lower esophageal ring.
7. The role of weight loss
Observational studies in overweight and obese patients show that weight loss leads to an improvement in GERD symptoms. Furthermore, reflux symptoms have been shown to worsen or improve over time concurrently with weight gain or loss, respectively. The HUNT study found that, among people with symptoms associated with GERD, a reduction higher than 3.5 BMI units was associated with a reduction or discontinuation of anti-reflux medication. weekly. On the other hand, whether weight loss can improve subjective or objective manifestations of reflux remains controversial. Furthermore, there is little data to determine whether weight loss can improve symptoms associated with gastroesophageal reflux disease such as laryngospasm.
8. Conclusion
The management of laryngeal reflux can be divided into lifestyle modification, medical therapy and/or surgery. Behavioral changes and lifestyle modifications are considered first-line treatments with the lowest chance of side effects. Weight loss, smoking cessation, alcohol avoidance, changes in dietary habits, and elevation of the head during sleep should be recommended for the patient. As for medical therapy, currently, treatment is focused on increasing the pH of the reflux substance, so it is advisable to start with PPIs twice daily for a period of 8-12 weeks. Tolerant patients with objective evidence (reflux monitoring) of ongoing reflux as the cause of symptoms should be considered for alternative therapies, such as visceral pain modifiers or endoscopic anti-reflux surgery.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
ReferencesIrene Martinucci, Nicola de Bortoli, Optimal treatment of laryngopharyngeal reflux disease, Ther Adv Chronic Dis. 2013 Nov; 4(6): 287–301. Altman K., Prufer N., Vaezi M. (2011) A review of clinical practice guidelines for reflux disease: towards creating a clinical protocol for the otolaryngologist. Laryngoscope 121: 717–723 [PubMed] [Google Scholar] Anderson J., Jhaveri M. (2010) Reductions in medications with significant weight loss with behavioral intervention. Curr Clin Pharmacol 5: 232–238 [PubMed] [Google Scholar] Bardhan K., Strugala V., Dettmar P. (2012) Reflux revisited: advancing the role of pepsin. Int J Otolaryngol 2012: 646901. [PMC free article] [PubMed] [Google Scholar]