This is an automatically translated article.
The article was written by MSc Vu Duy Dung - Doctor of Neurology, Department of General Internal Medicine - Vinmec Times City International Hospital.
Myeloma can be primary or secondary, benign or malignant. The incidence of primary tumors of the spinal cord is rare, and primary intramedullary tumors are the rarest form of spinal cord tumors, accounting for only about 10% of all spinal cord tumors.
1.What is an intramedullary primary myeloma? Primary tumors of the spinal cord are tumors that originate in the spinal cord, spinal nerve roots, and the dura mater, in contrast to spinal cord metastases, which originate from systemic cancers that have spread to the spine. Spinal myeloma is a rare but extremely dangerous disease, with a condition in which the spinal cord has tumors located in the spinal canal that cause nerve compression to the nerve structures in the spinal canal.
When the tumor grows larger, it will put pressure on the spinal cord and create neurological deficits in the lower spinal cord, causing the patient to have numbness, weakness, paralysis of the lower limbs or urinary incontinence. free...
2. Symptoms of primary myeloma Typical symptoms of primary myeloma include:
Weakness of limbs, sensory disturbances, sexual dysfunction, bladder and bowel disorders. Abnormal gait, and impairment in activities of daily living. Malignant spinal cord compression can eventually lead to paraplegia, quadriplegia, or even death.

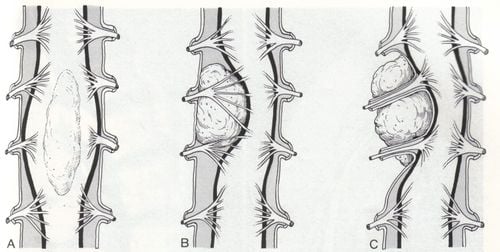
Classification of primary spinal cord tumors Primary spinal cord tumors can be classified according to their location as intramedullary, intradural extramedullary, or epidural. The incidence of primary tumors of the spinal cord is rare, and primary intramedullary tumors are the rarest form of spinal cord tumors, accounting for only about 10% of all spinal cord tumors.
3.1 Intramedullary Tumors Endometrial Tumors Diffuse gliomas Hairy astrocytomas Hemangioblastomas 3.2 Intramedullary extramedulomas Schwannomas Schwannomas Neurofibromas Neuroblastomas blood vessels Myxopapillary ependymoma 3.3 Epidural Tumors En plaque meningioma Schwannoma Mucinous papilloma of the intramedullary canal.
4. Classification of primary intramedullary myeloma and treatment methods 4.1 Diffuse glioma of the spine Diffuse gliomas include: Grade II and III astrocytoma, tumor Grade II and III oligodendroglioma, WHO grade IV glioblastoma, and disseminated midline glioma in children.
Diffuse astrocytomas, undifferentiated astrocytomas, and glioblastomas are now further genotyped as tumors with mutant IDH and primitive IDH. Gliomas carrying IDH mutations have a better prognosis.
The majority of diffuse and undifferentiated astrocytomas are IDH mutations, whereas only 10% of glioblastomas have IDH mutations. Lumpy gliomas almost always carry an IDH mutation and lose one copy of chromosomes 1p and 19q. This 1p/19q co-loss is a molecular marker of oligodendroglioma.
Diffuse astrocytomas are WHO grade II gliomas, diffuse infiltrates and are common in young people. The spine is the third most common site of diffuse astrocytomas after the tentacle and brainstem sites. Undifferentiated astrocytomas, glioblastomas, and oligodendrogliomas are rare in the spinal cord. One study reported that undifferentiated astrocytomas and glioblastomas accounted for 14% and 6% of all intramedullary astrocytomas, respectively.
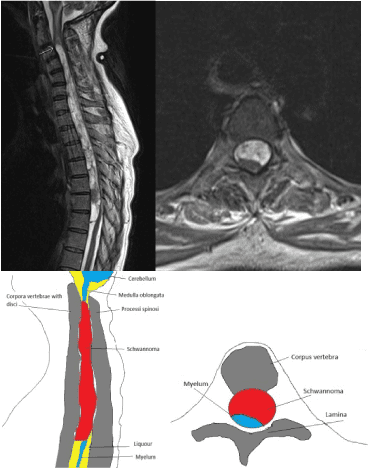
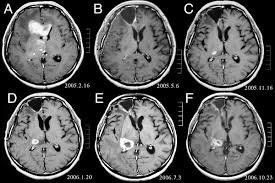
A new clinical entity according to the WHO classification is diffuse midline glioma, the H3 K27M mutation, which was originally named diffuse intrapontine glioma. These tumors are mainly seen in children but can also occur in adults. They have a diffuse pattern of growth and are located in the brain stem, thalamus, and spinal cord. Diffuse midline gliomas have a characteristic K27M mutation in the histone H3.3 gene H3F3A or, less commonly, in the histone H3.1 gene HIST1H3B. The majority of diffuse midline gliomas have an astrocytic phenotype. Molecular studies have shown that the K27M histone H3 mutation is mutually exclusive from the IDH1 mutation and EGFR amplification and is often associated with p53 overexpression, loss of ATRX, and monogenicity 10. Patients with neoplasms Diffuse midline glial in the spinal cord is older than in patients with pontine tumors. The radiographic differentiation of astrocytomas from endothelial medullomas is useful for preoperative planning and treatment.
On MRI, intramedullary medullomas are usually located on the central side of the spinal cord. They are often enhanced, show diffuse enhancement after gadolinium injection, are associated with bleeding, and are often empty of the pulp. Endometrial tubular tumors are co- or hypointense on T1 and hyperintense on T2. One-third of endothelial medullomas have a strongly hypointense border seen at the tumor poles due to accumulation of hemosiderin, known as the cap sign. It may be due to bleeding, which is more common in endothelial medullomas than in astrocytomas. Spinal cord astrocytomas are often eccentrically located, have faint boundaries, and are co- or hypointense relative to the spinal cord on T1 and hyperintense on T2. Cysts in the tumor and hollow pulp may be present but are less common than endothelial medullomas. The cap sign is not usually present in astrocytomas of the spinal cord. Spinal glioblastoma presents as a diffuse, infiltrative intramedullary mass with high signal intensity on T2 and heterogeneous enhancement on T1 after drug injection. The radiographic differences between endothelial medullomas and astrocytomas are valuable for preoperative planning. Total resection for astrocytomas is difficult because of its infiltrative nature. In contrast, classical endothelial medullary tumors are known to be well demarcated with adjacent normal spinal cord tissue and thus are easier to completely resect the tumor.
4.2 Hairy astrocytomas of the spinal cord Hairy astrocytomas are the most common primary brain tumor in children. The majority of hairy astrocytomas originate in the cerebellum, optic nerve, optic nerve, and hypothalamus. Meanwhile, hairy astrocytomas account for 11% of all childhood spinal cord tumors. Hairy astrocytomas are the most common CNS tumors associated with neurofibromatosis type 1. The majority of NF1-associated hairy astrocytomas occur in children. visual line. Hairy astrocytomas are usually relatively well-demarcated cystic tumors corresponding to WHO grade I. They have a biphasic histology – bipolar hairy cells tightly arranged together in bundles accompanied by acidophilic Rosenthal filaments, mixed with loose rough astrocytes. Bipolar hairy cells have long hair-like branches that can extend throughout the microscopic field, hence the term pilocytic. Rosenthal filaments are clear, glassy, acidophilic, spiral, cytoplasmic masses found in dense tissue. Such findings are common but not diagnostic of hairy astrocytomas and may be common in glioma or chronic glioma. The majority of ciliated astrocytomas have a variable fusion gene between the BRAF gene and the KIAA1549 gene (KIAA1549-BRAF) or, less commonly, a FAM131B-BRAF mediation gene. The BRAF V600E mutation is also commonly detected. Unlike the BRAF-mediated gene, which is found almost exclusively in hairy astrocytomas, the BRAF V600E mutation can be seen in polymorphic astrocytomas, gliomas, and graded gliomas. high.
Patients with hairy astrocytomas of the spinal cord often present with pain, sensory loss, and limb weakness. Involuntary radiculopathy and radiculopathy may be present, and symptoms are usually slow to progress. Children with a cervical medullary lesion may have nausea, vomiting, dysphagia, and nonspecific symptoms such as agitation and weight loss. The majority of these tumors are located in the cervical spinal cord, followed by the thoracic and lumbar spinal cord. In children, the tumor can extend the entire spinal cord from the cervical-medullary junction to the spinal cone.
On MRI, these whole spinal cord tumors have a strongly enhanced solid component and are often accompanied by a cyst and a wide tunnel at both ends. The tumor usually presents as a cystic lesion with a nodular enhancement in the wall. Cystogenesis can help distinguish hairy astrocytomas from diffuse, often non-follicular astrocytomas. Hairy astrocytoma is a rich vascular tumor with a glomerular vasculature but without epithelial hyperplasia. Thus, the tumor may present with irregularly thickened peripheral enhancement, irregular central cystic necrosis, or an irregularly heterogeneous hyperenhanced lesion, with an infiltrative border, thus resembling with a high-grade lesion. However, hairy astrocytomas diffuse readily, bright on ADC pulses and low signal on diffuse pulses, in contrast to high-grade gliomas, which may have limited diffusion (low signal on ADC pulses and high on the diffuse pulse).
Because of the location of the entire spinal cord, complete resection of the tumor is often not possible, and most patients have biopsies or incomplete resection. If there is a significant residual tumor, or if the tumor recurs after surgery, the patient will receive adjuvant therapy, usually radiation therapy.
4.3 Spinal cord hemangioblastoma Angioblastoma is a slow-growing and benign tumor, composed of neoplastic mesenchymal stem cells and an abundant network of small capillaries. They are commonly found in the cerebellum and brainstem.

Spinal cord hemangioblastoma presents with symptoms of pain, decreased sensation, and round muscle incontinence. Motor deficits appear late because this type of tumor is usually located in the posterior spinal cord.
The MRI findings of spinal hemangioblastoma are an enhanced mass with cystic and tunneling. Flow voids may be seen as nodules because of the presence of blood vessels. When the lesion is large or in the medulla oblongata, digitized background angiography may be needed to clearly visualize the feeding arteries as part of preoperative planning. The clinical outcome is excellent if the spinal hemangioblastoma is completely resected.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
SEE MORE
Spinal epidural tumor surgery - nerve root Spinal tumor can cause paralysis Epidural nerve root tumor surgery with vertebral reconstruction