This is an automatically translated article.
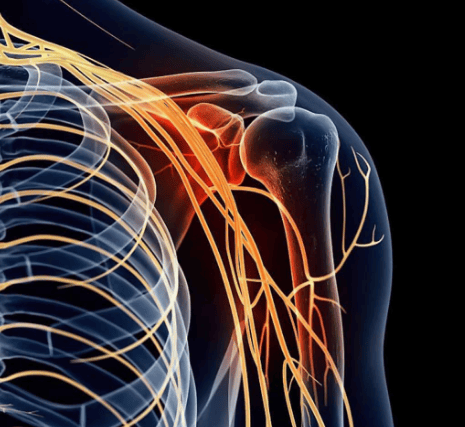
The article was professionally consulted with Master - Doctor Huynh An Thien - Department of Medical Examination and Internal Medicine, Vinmec Da Nang International General Hospital.Lumbar hip syndrome has 2 component syndromes including spinal syndrome and nerve root syndrome. Examination of the lumbar spine syndrome is a method performed to detect the symptoms of the two syndromes above, thereby making a definite diagnosis.
1. A brief overview of lumbar lumbar syndrome
Lumbar hip syndrome is a combination of both lumbar spine disease and sciatic nerve disease. The disease will be worse on cold and humid days.Some diseases often cause lumbar spine syndrome, including: Lumbar disc herniation, degenerative disc disease in the elderly, lumbar spondylosis, spondylolisthesis (due to congenital or trauma). , spondylitis, bacterial spondylitis (staphylococci, tuberculosis bacilli,...) or trauma (lumbar spine fracture, pelvic fracture, trauma directly affecting the sciatic nerve) ),...
People with lumbar lumbar syndrome often present as spinal syndrome and nerve root syndrome with the following characteristic symptoms:
Spine syndrome: Low back pain, usually only in certain vertebrae, can be severe or dull, sudden, or comes on after an injury. In addition, the patient also has a deformed spine (change in physiological curves, decreased or lost flexion, hunchback, scoliosis) and reduced range of motion of the lumbar spine (limited bending). , supine, tilt or rotate the spine); Nerve root syndrome: Nerve root pain that radiates along the path of the nerve root, aching pain, pain that increases when walking, standing, coughing or sneezing but markedly relieved at rest. There are cases of pain in all positions, affecting the ability to walk, work and live.

2. How to diagnose low back syndrome?
Examination for lumbar lumbar syndrome is the simultaneous examination of both sub-components of this condition, the spinal syndrome and the radiculopathy. Specifically:2.1 Examination of spinal syndrome First, the doctor asks the patient to stand upright, then checks according to the following procedure:
Assess the shape of the spine: The doctor checks whether the patient's spinal axis is it straight, is it skewed or crooked to the left or right; physiological curvature (lumbar arch) is normal or reduced, lost or reversed; Finding pain points in the spine: The doctor presses or knocks on the spines of the vertebrae to find the pain points in the spine (injured vertebrae will be more painful than other normal vertebrae); Evaluation of paravertebral muscle tone: The doctor looks from behind the patient's back to see if the paraspinal muscle mass on both sides is balanced, then adjusts to check the muscle tone of those two muscle blocks to see if they are equal. if not, assess which side has increased muscle tone; Checking the mobility of the spine: The doctor checks the patient's spinal motor functions such as bending, tilting, tilting and rotating the spine: Lumbar flexion: The doctor uses a measure of the curvature of the spine. belt. The normal waist flexion is 18mm - 30mm. If the examinee has pain with lumbar flexion or limited flexion, this is a sign of pathology; Bend: Can be examined by finger-ground method or based on Schober index. With the finger-ground distance test method, the doctor makes the patient stand upright, the legs close together, and then asks the patient to bend as much as possible, straighten the legs, raise both arms straight to the ground, and then measure the distance from the fingers. the patient's middle to the ground (people with a healthy spine usually have zero finger-to-ground distance - that is, the finger can touch the ground, while patients with a herniated disc with nerve root irritation have no fingers do not touch the ground). With the Schober index method, the doctor first makes the patient stand upright, determines the spinous process of the S1 vertebra, and re-marks it. From this point, the doctor measures up 10cm, marks the 2nd point. After that, the doctor makes the patient stoop to the maximum, both legs are stretched at the knee joint, measure the distance between the 2 points above (in the stooped position). of the patient). Schober index = 1st measurement / 2nd measurement. In normal people of the young age group, Schober index is about 14/10 - 15/10. In patients with lumbar lumbar syndrome - this indicator decreases; Spinal rotation and tilt: The doctor uses a measure of rotation and inclination. The spine of a normal person can be tilted 29 - 31° to both sides and rotated about 30 - 32°. If the patient has pain on tilting or turning or the angle of inclination and rotation is limited, it indicates disease.

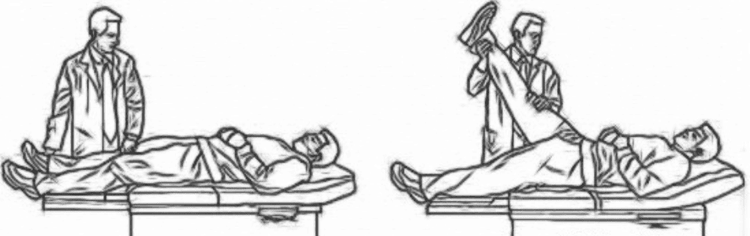
Paravertebral pain score: The physician has the patient stand or lie down in a comfortable position. Then, the doctor examines the pressure on the paravertebral line (about 2cm from the spine axis to the left and right) at the level of the midpoint of the interspinous distance. When pressed, the damaged nerve roots will feel pain; Lasegue sign: The doctor puts the patient in a supine position, with both legs stretched out in a comfortable position. Next, the doctor uses his one hand to hold the ankle, the other hand is placed on the patient's knee, keeps the patient's leg straight and examines in the following 2 steps: Step 1: The doctor elevates the patient's leg (in a standing position) straighten) up off the bed, toward a 90° angle until the patient complains of pain, stretches along the back of the leg, then stops. Next, determine the angle between the patient's foot and the bed surface - this is called the Lasegue angle. Specifically, if the leg is raised to 45° and the patient complains of pain, the Lasegue angle is 45°; Step 2: The doctor keeps that angle and flexes the patient's leg at the knee joint. The patient will no longer have pain along the back of the leg. Examine the patient's legs in turn. Evaluation: A normal healthy person has a Lasegue angle of 90°. The positive Lasegue sign manifests at the same time in 2 factors: the patient feels pain when the leg is not perpendicular to the bed surface (step 1) and when the patient's leg is folded, the pain disappears (step 2); Cross Lasegue sign: When the doctor looks for Lasegue sign in the healthy leg, the patient has increased pain in the affected leg; Bell sign: The doctor has the patient lie down or stand in a comfortable position. Then, the doctor presses on the points as in the manipulation of the spine pain point. The bell sign gives a positive result when the patient feels pain spreading along the path of the ipsilateral sciatic nerve to the lower leg; System of Valleix points: The points through which the sciatic nerve passes, including the midpoint of the gluteal fold, the point between the situ and the trochanter, the midpoint of the back of the thigh, the midpoint of the hamstring. When examining low back syndrome, the doctor uses his finger to press on the upper points. If the sciatic nerve is damaged, the patient will feel a sharp pain at these points on examination; Dejerine's sign: The patient has pain in the lower back when coughing, sneezing; Neri's sign: When examining the patient, stand up straight, then bend over, raise both hands to touch the ground and keep both knees straight. Positive Neri sign when the patient feels pain along the affected leg and the leg is contracted at the knee joint; Siccar sign: The doctor puts the patient in a comfortable supine position and straightens the legs. The doctor manipulates the examination such as checking the Lasegue sign in step 1, lifting the patient's foot off the bed, until the patient has pain, then stops, flexes the foot on that side towards the pubic side. Positive Siccar sign if the patient feels increased pain along the dorsal side of the leg being examined;
Movement disorders: check the motor function of L5 and S1 roots because these two roots are very often injured in cases of disc herniation: L5 root: Chi Coordination of movement of the anterior tibial muscle group, the function of flexing the foot and flexing the 1st and 2nd toes to the pubic side. During examination, the doctor checks the strength of the flexor muscles of the foot and flexes the toes 1 - 2 towards the pubic side on both sides of the leg; Have the patient stand on his heels. In a person with L5 root damage, the patient has difficulty or no standing on the affected heel side; S1 root: Controls movement for the posterior calf muscle and has the function of extending the foot. During the examination, the doctor checks the strength of the extensor muscles of the foot or has the patient stand on the tip of the foot. In a person with an S1 root lesion, the patient has difficulty or no standing on the tip of the affected foot; Reflex disorder: Check the reflex function of nerve roots, especially: femoral-scrotal reflex (root L1, L2), tendon reflexes of quadriceps tendon (root L3, L4) and reflexes Achilles tendon (S1 root); Sensory disturbances: Perform sensory function tests of the sacral nerve roots. The L4, L5 and S1 roots need to be examined more carefully because it is directly related to herniated disc pathology; Neurovegetative-nutritional disorders: Check the function of temperature regulation, vasomotor nutrition and sweating status of the skin bands. It is important to check for muscle atrophy, identify which muscle atrophy to help identify nerve root damage.

Vinmec International General Hospital is a high-quality medical facility in Vietnam with a team of highly qualified medical professionals, well-trained, domestic and foreign, and experienced.
A system of modern and advanced medical equipment, possessing many of the best machines in the world, helping to detect many difficult and dangerous diseases in a short time, supporting the diagnosis and treatment of doctors the most effective. The hospital space is designed according to 5-star hotel standards, giving patients comfort, friendliness and peace of mind.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.