This is an automatically translated article.
The article is written by Master, Doctor Mai Vien Phuong - Department of Examination & Internal Medicine - Vinmec Central Park International General HospitalUlcerative colitis (UC) is a chronic, nonspecific, or recurrent inflammatory bowel disease. The colon is considered to be the major target organ of ulcerative colitis, whereas upper gastrointestinal (UGI) manifestations are infrequent. Recently, emerging evidence suggests that ulcerative colitis causes complications in mucosal damage to the esophagus, stomach, and duodenum.
1. Overview
Ulcerative colitis (UC) is a chronic, nonspecific, or recurrent inflammatory bowel disease. The colon is considered to be the major target organ of ulcerative colitis, whereas upper gastrointestinal (UGI) manifestations are infrequent. Recently, emerging evidence suggests that ulcerative colitis causes complications in mucosal damage to the esophagus, stomach, and duodenum. However, the upper gastrointestinal tract manifestations associated with ulcerative colitis are diverse and often insidious or masked. Furthermore, the endoscopic and microscopic features of the upper gastrointestinal tract complicated with ulcerative colitis are nonspecific. Therefore, upper gastrointestinal involvement may be overlooked by many clinicians.
2. Gastroduodenal mucosal damage in patients with ulcerative colitis
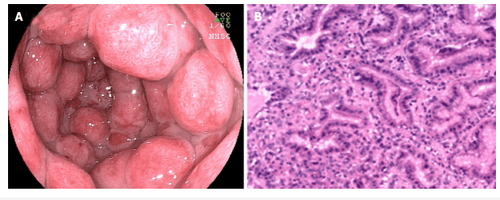
2.1. Gastric and duodenal lesions Ulcerative colitis complicated by gastrointestinal injury was first reported by Sasaki et al. Multiple erosions and granular changes in the great curvature of the stomach wall and descending part of the duodenum have been demonstrated. Histologically, they confirmed clear inflammatory cell infiltration and abscesses in the stomach and duodenum. Thereafter, there is increasing evidence of gastrointestinal mucosal damage in patients with ulcerative colitis.
More recently, the concept of peptic ulcer disease (UGDL) or gastroduodenitis associated with ulcerative colitis has been proposed. Diagnostic criteria for peptic ulcer disease include: Lesions may improve after treatment for ulcerative colitis and a pathological examination similar to ulcerative colitis. However, the diagnostic criteria are not rigorous enough because of rare reports. Several factors have been shown to be major risk factors for ulcerative colitis-associated gastritis, including extensive colitis, use of lower doses of prednisolone, and occurrence of pouchitis. jejunostomy, postcolectomy colitis, and longer postoperative time
Previously, FEG was described as a specific diagnostic marker for patients with Crohn's disease. However, different opinions have also been suggested. The academics also found that FEG could be seen in 20.8% of children with ulcerative colitis. Although, it remains uncertain whether the utility of FEG can distinguish Crohn's disease from ulcerative colitis in adults, it is unreliable in children. Basal and patchy inflammation is the second pattern of gastritis, consisting of a loose mixture of lymphocytes, eosinophils, mast cells, and plasma cells. These cells are found in the buffer between the deepest glands and the muscular lining. Furthermore, plasma cell surface is the third most common pattern of gastritis. It is considered as a diffuse band of plasma cells in the superficial stroma adjacent to the pits and necks.
Chronic diffuse gastritis also seems to be a common feature in gastric biopsies from individuals with ulcerative colitis. In a recent study it was suggested that active inflammation of the stomach and/or duodenum may be associated with drug-resistant ulcerative colitis. Notably, erosive or ulcerative lesions complicated with ulcerative colitis are infrequent and granulomas are always absent. In terms of gross and endoscopic features, gastritis associated with ulcerative colitis is characterized by diffuse granular or brittle mucosa, as well as atrophic lesions. For the differential diagnosis, patients with ulcerative colitis present with mild chronic inflammation with or without neutrophils and a specificity problem, which may be correlated with environmental factors and regimens. eat and drink. Inflammatory cell infiltration observed in Helicobacter pylori-associated gastritis and Crohn's disease-associated chronic superficial gastritis is more dense and diffuse than in ulcerative colitis.
2.2. Duodenal ulcer is not usually considered the target organ of ulcerative colitis. However, as early as the 1960s, chronic duodenitis associated with ulcerative colitis was first demonstrated. Later, new evidence emerged suggesting the presence of chronic duodenitis associated with ulcerative colitis. However, it is still infrequent. Indigestion is the most common symptom of chronic duodenitis associated with ulcerative colitis, but it is often covered by symptoms of ulcerative colitis. Notably, most patients with symptomatic duodenitis present with severe colitis, in some cases requiring colectomy. More interestingly, some individuals with ileostomy-anal sacs also develop this pouchitis. The only type of upper GI inflammation in individuals with ulcerative colitis is diffuse chronic duodenitis, which occurs in 10% of patients with duodenal biopsies, and combined resection occurs in 40% of patients with ulcerative colitis. Ulcerative colitis has inflamed pouches.
The endoscopic findings reported in patients with symptoms are varied and include diffuse edema, granulomatous, mucosal thinning and ulceration, etc. Furthermore, microscopic features of duodenitis associated with ulcerative colitis include dilated mucosa with diffuse inflammatory infiltration of monocytes and neutrophils, glandular deformity, and erosion. or ulcer. Accordingly, duodenal IELs with Crohn's disease 3 (+) and Crohn's disease 8 (+) or stromal mononuclear cells may be present in a wide range of patients with ulcerative colitis.
In summary, duodenitis complicated with ulcerative colitis is often identified by its specific microscopic and capillary features as well as its overlap with celiac disease, duodenitis, and associated duodenitis. related to drugs. However, clinical awareness should be considered when diagnosing ulcerative colitis, especially if the patient has had prior surgical resection because of extensive and severe colitis or if the patient has concomitant pouchitis or inflammatory bowel disease. intestine .
3. Esophageal mucosal injury in patients with ulcerative colitis
3.1. Frequency of inflammatory bowel disease and associated upper gastrointestinal tract lesions Millions of people worldwide are affected by ulcerative colitis, which is already considered a global disorder. The prevalence of ulcerative colitis has been increasing since the mid-20th century. However, pediatric IBD patients are generally thought to have an upper gastrointestinal tract involvement more commonly than adult patients. This difference may be because upper gastrointestinal endoscopy is performed less frequently in asymptomatic adult patients with IBD than in their pediatric patients. Patients with ulcerative colitis receive targeted treatment at a variety of institutions, from community and public hospitals to clinics.
However, upper gastrointestinal involvement may go unnoticed by the attending physician due to lack of knowledge about gastrointestinal injury, which would raise concerns during the treatment of inflammation ulcerative colitis. In fact, there are no established criteria or criteria for patients with ulcerative colitis who present with endoscopic gastroscopy (FGDS) lesions. Because the clinical background of these patients with ulcerative colitis-associated upper gastrointestinal tract lesions has not been fully and precisely established. Specific management may be required for patients with upper gastrointestinal tract involvement associated with ulcerative colitis.
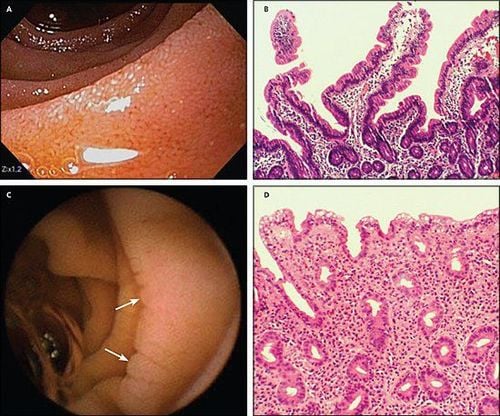
3.2. Esophageal mucosal lesions Traditionally, ulcerative colitis has been considered to be a disease of the colon distinct from self-limiting terminal ileitis. However, in recent years, the initial prevalence of esophageal disease associated with ulcerative colitis has been 12%-50%, while the prevalence is as high as 70% to 90% in individuals with ulcerative colitis. Crohn's (CD). These numbers may underestimate the prevalence of the disease due to the difficulty of accurate diagnosis and the lack of standard endoscopy in asymptomatic individuals with ulcerative colitis. It is difficult to diagnose the esophageal complications of ulcerative colitis because these complications can manifest as diverse esophageal symptoms, such as erosive esophagitis or esophageal stricture, which have many common with other common esophageal diseases. In addition, the microscopic manifestations and characteristics of esophageal complications with ulcerative colitis are often unidentified. Although the incidence of esophageal disease complicated with ulcerative colitis is lower than that of esophageal disease complicated with Crohn's disease, it is still important to identify esophageal disease associated with ulcerative colitis.
3.3. Esophagitis The first case of esophagitis was reported by Margoles et al. in 1961. The occurrence of esophagitis was described more frequently in pediatric patients than in adults. However, endoscopic and histological features were indeterminate or nonspecific. In addition, it is difficult to evaluate for other unrelated disorders, such as reflux disease, medication, or candidiasis. Lymphocytic esophagitis (LE) is defined as a large number of pericapillary lymphocytes (PLs) or intraepithelial lymphocytes (IELs) with no significant granulocytes (neutrophils and white blood cells). eosinophils), and lymphocytic esophagitis was initially shown to be an upper gastrointestinal manifestation in children with IBD. Lymphocytic esophagitis has been reported in 7% of pediatric patients with ulcerative colitis, and mucosal lesions (oedema or keratitis) are commonly seen in patients with ulcerative colitis. However, no significant difference was found between IBD and non-IBD controls. In contrast, a previous study suggested that PL found in lymphocytic esophagitis could be a marker for disease activity in IBD. The diagnosis of lymphocytic esophagitis in patients with ulcerative colitis should be differentiated from candidiasis, lichen planus esophagitis, and lichenoid esophagitis. Granulomatous esophagitis has been reported in patients with Crohn's disease but not in patients with ulcerative colitis. Histological criteria for granulomatous esophagitis include chronic granulomatous disease, common variable immunodeficiency, and infection.
Furthermore, a previous analysis also showed that there was a statistically significant inverse association between eosinophilic esophagitis and Crohn's disease or microscopic colitis, but not ulcerative colitis. .
3.4. Esophageal ulcers There are relatively few reports of esophageal ulcers associated with ulcerative colitis. To date, only 20 cases of esophageal ulcers (including ours) were associated with ulcerative colitis. The clinical features of these patients are listed in Table 2. This is a perforated ulcer and is usually found in the middle of the lower esophagus. According to previous findings, esophageal ulcers are more commonly seen in younger people than in the elderly. In addition, patients often have complicated esophageal ulceration at the onset of colitis or when it recurs. However, the endoscopic manifestations of ulcerative colitis patients with esophagitis are not the same as those of gastroenteritis associated with ulcerative colitis (GDUC).
Gastritis associated with ulcerative colitis is characterized by granular and friable mucosa, but conversely, esophageal ulcers due to complicated ulcerative colitis are perforated and frequently occur. mid to lower esophagus. Pathologically, only nonspecific inflammatory cell infiltration was demonstrated in all reported cases, without any ulcerative colitis-specific features. However, histologically, an association between esophageal ulceration and ulcerative colitis was not established. Esophageal lesions are still effective in the treatment of ulcerative colitis.
In addition, most patients with ulcerative colitis with ulcerative esophagitis have other extra-gastrointestinal manifestations, including ocular trauma, skin disorders, and peripheral arthritis. However, the underlying pathological mechanisms have not yet been identified. Therefore, esophagitis complicated by ulcerative colitis is particularly uncommon. They can occur as an extra-gastrointestinal manifestation in most cases of ulcerative colitis. Pathological findings of esophageal lesions did not identify ulcerative colitis. Therefore, a comprehensive diagnosis is needed to rule out infections and drug-related diseases.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
References
Sun Y, Zhang Z, Zheng CQ, Sang LX. Mucosal lesions of the upper gastrointestinal tract in patients with ulcerative colitis: A review. World J Gastroenterol 2021; 27(22): 2963-2978 [DOI: 10.3748/wjg.v27.i22.2963]