This is an automatically translated article.
Unlike erythrocytes, leukocyte-poor red blood cells are characterized by a very low or absent white blood cell count. Accordingly, the risk of blood transfusion accidents is minimized, especially in patients who need multiple blood transfusions or have special backgrounds.1. What are leukocyte-poor red blood cells?
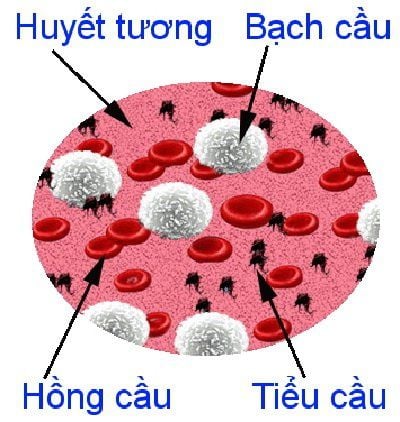
After the principles of safe blood transfusion were introduced, many patients were saved from acute blood loss. However, if because of hematological diseases, the red blood cell line is suppressed and the patient requires a prolonged blood transfusion to maintain life, repeated blood transfusions will contain more and more risks for the patient. patients, increasing over time.It is hypothesized that transfusions of blood containing white blood cells may cause side effects through multiple mechanisms. White blood cells can cure infectious diseases on their own, and some pathogens are more concentrated in white blood cells than in the rest of the blood product. It has also been hypothesized that the donor white blood cells might suppress the recipient's immune system by interacting with it. Therefore, the idea of the need for a blood transfusion that only needs red blood cells, without or minimizing the number of white blood cells, was born.
To meet this need, clinical hematologists have researched and produced leukocyte-poor red blood cells. This is a concentrated mass of red blood cells, but an extra step is to remove the white blood cells with a white blood cell filter. Leukocyte filtration must be performed within 72 hours of blood collection from the donor. The leukocyte-poor red blood cells are then packaged under a volume of 120ml per unit provided that a very low white blood cell count is required, less than one million cells per unit. The average hemoglobin (Hct) ratio of leukocyte-poor red blood cells can be as high as 60 to 70%.

Khi dòng hồng cầu bị ức chế và người bệnh đòi hỏi cần được truyền máu kéo dài để có thể duy trì sự sống,
2. In which case are leukocyte-poor red blood cells used?
Acceptable reasons for using leukocyte-poor red blood cell preparations :Prevention of immunostaining for HLA antigens Prevention of formation of non-hemolytic transfusion reactions with repeated transfusions Minimization leukemic reactions (anti-leukocyte antibodies, lymphocytes, mediators) There is a need for blood transfusion for the fetus in utero, the neonate, or the person with congenital or acquired immunodeficiency Prevention of CMV transmission or the risk of disease transmission where the agent is located in leukocytes Accordingly, in practice, the main indication for the use of leukocyte-poor red blood cells is in patients with marrow transplantation, organ transplantation. any organ transplant preparation to minimize the patient's immune response. Also, in patients with more than two transfusion-related fevers, leukocyte-poor red blood cells should be used when improvement in hemoglobin is required.
In addition, when a large number of red blood cells are required, multiple transfusions should be given to patients with thalassemia major or other congenital anemia such as sickle cell anemia. , marrow failure, leukemia...

Hồng cầu nghèo bạch cầu được truyền cho bệnh nhân
3. How to prepare and use leukocyte-poor red blood cells?
Leukocyte-poor red blood cells are prepared by removing 70-85% of white blood cells by centrifugation, filtration or ultraviolet irradiation. The effect is different in each method.Among them, filtration is the best method to reduce white blood cells. Currently, there are many different white blood cell filters on the market. The general principle is to combine with physical filtration and adsorption filtration to achieve the highest efficiency, done by passing the entire unit of blood through the filter. Inside the filter are a lot of densely packed fibers, white blood cells will be trapped between, only red blood cells pass through. The results obtained are only red blood cells or mixed with a few white blood cells, but the number is very small.
Then, the leukocyte-poor red blood cell units are stored and ready to use like other blood products. In particular, the blood distribution process, blood group testing and blood compatibility between the blood bag and the patient's blood are always strictly followed.
In the case of medical units and hospitals that do not have ready-made and stocked leukocyte-poor red blood cells, if there is an acute indication, a temporary preparation of leukocyte-poor RBCs can be made at the hospital. bed by using concentrated red blood cells to pass through a leukocyte filter. In addition, the departments need to have ready the means of handling blood transfusion accidents to immediately respond when necessary.
In a nutshell, leukocyte-poor red blood cells are preparations containing only red blood cells with very little or no white blood cells. It is this condition that will limit the risk of reactions and transmission of infectious agents through the white blood cell route during blood transfusion, especially beneficial for patients with serious diseases that cannot be treated. requires a lifelong blood transfusion.
SEE ALSO:
Elevated white blood cells warn of what disease? What is the number of white blood cells in the body? What do you know about the rarest blood types?