This is an automatically translated article.
The article was written by a Doctor of Hematology - Blood Transfusion - Laboratory Department - Vinmec Ha Long International Hospital.1492 : In Rome, Pope Innocent VIII suffered a stroke, he became weak and comatose. The doctor recommended a blood transfusion as a treatment for the Pope's illness. Due to underdeveloped Medicine, the Pope's condition did not improve and died later that year.
1615: Andreas Libavius describes his blood transfusion technique. However, his technique is not fully published.
1628: English physician William Harvey (1578-1657) describes the function of the heart and the circulation of blood. He showed that the heart is a pump and that the contractions of the heart push blood into the arteries and that blood returns to the heart after circulating through the veins. Thus, blood circulates throughout the body. Harvey deduced that the function of the valves is to prevent blood from flowing back into the veins.
1665: First recorded blood transfusion. Dr. Richard Lower (Oxford) experimented with animal blood transfusions (transfusion of blood from dogs to dogs) and performed a blood transfusion from animals to humans 2 years later. Dogs receiving blood transfusions are kept alive by transfusions of blood from other dogs.
1667 : Jean-Baptiste Denis in France reports a successful blood transfusion from sheep to humans.
1678 : Animal-to-human blood transfusion was tried in various ways, but was unsuccessful and was later banned by the Paris Society of Physicians because of the many complications that resulted in death.
1795: American doctor in Philadelphia, Philip Syng Physick, performed the first human blood transfusion, although he did not specifically publish it.
1818: James Blundell, an English obstetrician, successfully performed a human blood transfusion in a patient with postpartum haemorrhage. The blood donor is the patient's husband, he takes a small amount of blood from the husband's arm, uses a syringe, and transfers it directly to the wife. Between 1825 and 1830, he performed 10 blood transfusions, 5 of which proved beneficial to the patient, and the results were published. He also invented various tools for performing blood transfusions.
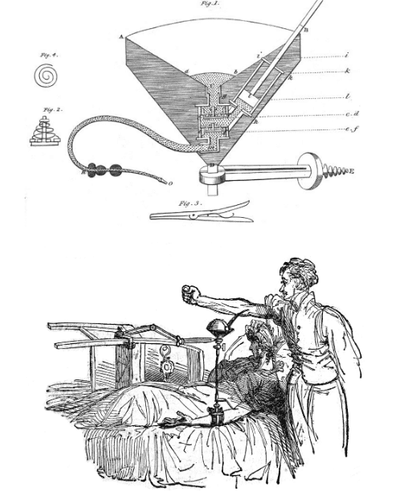
Hình 1: Các công cụ truyền máu của James Blundell
1840: In London, England, Samuel Armstrong Lane, assisted by consultant Dr. Blundell, successfully performed the first blood transfusion to treat hemophilia.
1867 - British surgeon Joseph Lister uses disinfectants to control infection in blood transfusions.
From 1873-1880 - During these years, American doctors recorded, passed milk (from cows, goats) to humans.
1884 - Infusion of saline milk substitute as a “blood substitute”, due to increased frequency of adverse reactions to milk.
1901 - Karl Landsteiner, an Austrian doctor, the most important individual in the field of blood transfusion, for the first time 3 human blood types were recorded A, B and O.
Hình 2: Bác sĩ Karl Landsteiner
1902 : The 4th major blood group is the AB blood type of humans as noted by A.Decastrello and A. Sturli.
1907 : Hektoen suggested that the safety of blood transfusion could be improved by performing cross-matching between donor and patient blood to rule out incompatible mixtures. Reuben Ottenberg first transfused blood according to blood type and performed cross-matching. Ottenberg also applies Menden's law to blood types, and O is the most commonly recognized group.
1908: French surgeon, Alexis Carrel proposes a method to stop blood clotting. His method entails connecting the donor artery directly to the recipient's vein through the suture of the incision. He first used the technique to save the life of a friend's son with three blood donors. This procedure was not feasible for blood transfusion, paving the way for the later successful organ transplantation, for which Carrel received the Nobel Prize in 1912.
1908 : Carlo Moreschi noted the Antiglobulin reaction.
1912: Roger Lee, a physician at Massachusetts General Hospital, along with P. D. White, formulate and develop the "Lee-White" clotting time. Lee went on to demonstrate that blood from all groups could be transfused into patients with group AB.
1914: New anticoagulant that prolongs anticoagulation, Natricitrate is discovered, allowing for longer preservation of blood.
1915 : At Mt. Sinai in New York City, Richard Lewisohn is credited with using Natricitrate as an anticoagulant, transforming the former blood transfusion routine into today's basic blood transfusion and Muscle Blood Bank operations. version has been formed. Furthermore, at the same time, R. Weil demonstrated the feasibility of cryopreservation as a form of anticoagulation.
1916: Francis Rous and J. R. Turner introduce a glucose citrate solution that can store blood for several days after a blood draw. In addition, in 1915 Lewisohn discovered this to allow blood to be stored in containers for later transfusion and the vein-to-vein method was introduced. This discovery also directly led to the establishment of Britain's first "blood stockpile" during World War I. Oswald Robertson is credited as the author of this "blood stock".
1925 : Karl Landsteiner, then working in New York City, in partnership with Phillip Levine, discovered three blood types: M, N and P.
1926 : British Red Cross establishes blood transfusion services the first in the world.
3030: Karl Landsteiner, the most important figure in Transfusion Medicine, discoverer of the first three human blood types, receives the Nobel Prize in Medicine.
1932 : The first facility as a blood bank was established in Leningrad Hospital, Russia.
1937: Bernard Fantus, director of treatment at Cook County Hospital in Chicago, Illinois (USA), establishes the first hospital blood bank in America. With a Hospital laboratory capable of holding and storing donor blood, Fantus calls it a "Blood Bank". Within a few years, Hospital and community blood banks began to be established throughout the United States. In the United States, some of the earliest recorded Blood Banks are in Cincinnati, Miami, New York, and San Francisco.
1939 and 1940: The Rh blood group system was discovered by Karl Landsteiner, Alex Wiener, Philip Levine and R. E. Stetson and quickly recognized as the cause of the majority of subsequent transfusion reactions. Called the Rhesus (Rh) system, a reliable test for this Rh group was established, transfusion reactions became rare. Determining the Rh factor, besides ABO, was an important breakthrough in Blood Bank.
Hình 3: Nhóm máu ABO, Rh
1940: Edwin Cohn, a professor of biochemistry at Harvard Medical School, developed a cold fractionated ethanol, the process of separating plasma from other components of blood. Albumin, a protein with strong osmotic properties, plus gamma globulin and fibrinogen has been isolated and ready for clinical use. The effectiveness of using albumin in blood transfusion was first demonstrated by John Elliott.
1941 : Isodor Ravdin, a renowned surgeon from Philadelphia, effectively shocks victims of Pearl Harbor with Cohn's albumin. Injected directly into the bloodstream, albumin absorbs fluid from surrounding tissues, preventing the collapse of blood vessels, which is associated with shock.
1943: J. F. Loutit and P. L. Mollison introduce acid citrate dextrose (ACD) solution, which reduces the volume of anticoagulants, allowing for larger blood volume transfusions and longer blood storage.
1943 : P. Beeson published a blood transfusion accident related to hepatitis.
1945: Coombs, Mourant and Race describe the use of Antihuman Globulin "Coombs Test" to identify abnormal antibodies.
1947: The Association of American Blood Banks (AABB) is established to "advance the common goals of American blood banks and blood donation."

Hình 4: Ngân hàng máu
1949 and 1950: The blood collection system in the US has grown to about 1,500 Hospital blood banks, 46 Community Hematology centers and 31 regional Red Cross societies in the US.
1950: The use of glycerol as a preservative to freeze red blood cells becomes widespread.
1950: Carl Walter and W. P. Murphy, Jr., introduce plastic bags for blood collection. Replace fragile glass bottles with plastic bags. This technical development entails the development of safer and easier collection systems that prepare multiple blood components from a single unit of whole blood.
1951: AABB (American Association of Blood Banks) establishes a central system of centralization, supply, and exchange between blood banks in the United States.
1953 : Development of refrigerated centrifuges for the preparation of therapeutic blood components.

Hình 5: Các chế phẩm máu
1954: Cryoprecipitate (now AHF) is developed for people with hemophilia.
1954-1958 : A product made from plasma was developed to treat diseases such as chickenpox.
1959: Max Perutz of the University of Cambridge deciphers the molecular structure of hemoglobin, the molecule that transports oxygen and gives red blood cells color.
1960 : A. Solomon and J. L. Fahey first report on therapeutic dialysis.
1961: The role of platelet concentrate in reducing mortality in hemorrhagic cancer patients is recognized.
1962: The first concentrated Antihemophilic Factor (AHF) for the treatment of hemophilia patients was developed through fractional distillation.
1962 : In the US there are about 4,400 Hospital blood banks, 123 Community Hematology centers and 55 Red Cross centers, which collect six million units of blood per year.
1964: Plasma extraction is introduced as a means of fractional plasma collection.
1967: Rh immunoglobulin was introduced commercially to prevent Rh disease in infants of Rh-negative mothers.
1969: S. Murphy and F. Gardner demonstrated the feasibility of storing platelets at room temperature, revolutionizing platelet transfusion therapy.
1971 : Hepatitis B surface antigen (HBsAg) testing in blood donors started in the US.
1972: Platelet extraction “Apheresis” was used to separate platelets.
1979 : A new anticoagulant, CPDA-1, prolongs the storage life of blood and blood cells to 35 days, enhances blood supply and facilitates blood sharing between blood banks .
Early 1980s: Doctors began to receive special training in blood transfusion and became actively involved in patient care.
1983: Newly introduced red blood cell nutrient, extending blood storage time to 42 days.
1985 : The first blood screening test for HIV is licensed and performed by the American Blood Bank.
1987: Two indirect tests to screen for hepatitis C are developed and performed: anti-HBc and liver enzyme alanine (ALT).
1989 : In the US, the first screening for HTLV-I virus (anti HTLV-I) was performed in blood donors.
1990 : Screening test for hepatitis C (non-A, B hepatitis).
1992 : Screening test for anti-HIV-1 antibodies and HIV-2 antibodies.
1996 : HIV p24 antigen test.
1999: Nucleic Acid Amplification Testing (NAT) used in blood screening is FDA approved. NAT directly detects the genetic material of viruses such as hepatitis C and HIV.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
The article references the source:
THE HISTORY OF BLOOD TRANSFUSION AND BLOOD TRANSFUSION MEDICINE. http://www.bloodbook.com/trans-history.html.
The History of Blood Banking