This is an automatically translated article.
The article was written by MSc Tong Diu Huong - Radiologist, Department of Diagnostic Imaging - Vinmec Nha Trang International General HospitalLymphedema may be primary or secondary, resulting from surgery or other pathological processes. The disease can be disfiguring due to local swelling and induration. Treatment can be difficult in many cases.
1. What is Lymphedema?
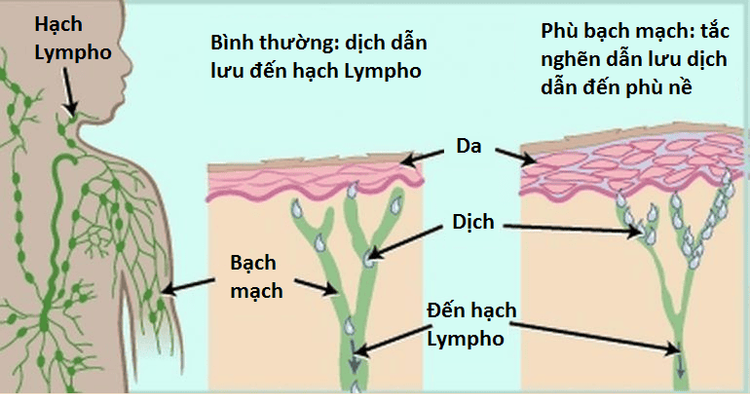
Lymphedema is a pathological accumulation of fluid in soft tissues as a result of poor lymphatic drainage, leading to inflammation, adipose tissue hypertrophy, and fibrosis.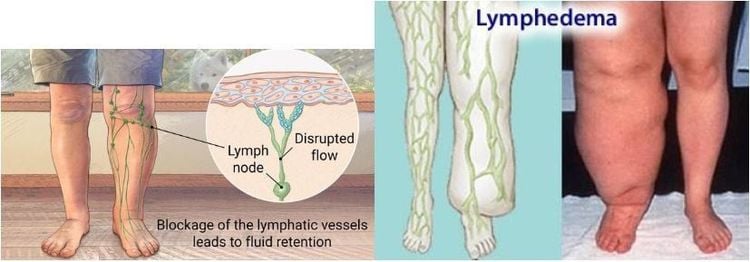
2. Epidemiology
Most cases of primary lymphedema are sporadic, with the remainder being hereditary or associated with other congenital pathologies.
The incidence of secondary lymphedema has been increasing in recent years due to an increase in the number of patients undergoing breast and pelvic surgery with or without radiation therapy. In fact, in developed countries, lymphedema secondary to iatrogenic causes accounts for the majority of cases.
3. Pathology
Lymphedema occurs due to the accumulation of fluid in the interstitial space and in the lymphatic system in the skin and subcutaneous tissue. This then stimulates fibroblasts, keratinocytes, and adipocytes, resulting in the deposition of collagen and glycosaminoglycans in the skin and subcutaneous tissue, leading to skin hypertrophy and destruction of elastic fibers.
Traditionally, it has been defined as interstitial edema and protein accumulation due to defects in the lymphatic drainage system. Recent findings suggest that interstitial protein levels may be low in some types of lymphedema.
4. Classification
Lymphedema is classified as primary and secondary.
4.1. Primary Lymphedema Due to a defect in the lymph vessels or lymph nodes themselves. Hereditary lymphedema and genetic related conditions. Chromosomal aneuploidy: Klinefelter syndrome, Turner syndrome, Trisomy 21 (Down syndrome), Trisomy 13 (Patau syndrome), Trisomy 18 (Edwards syndrome).
+ Morphological disorders: Milroy disease, Klippel-Trénaunay syndrome, Noonan syndrome, neurofibromatosis type 1, lymphedema-hypothyroidism syndrome, Meige disease.
4.2. Secondary lymphedema arises due to obstruction or disruption of the entire lymphatic system (including lymph nodes and lymph vessels).
Lymph nodes : Due to physician's intervention: lymphatic fibrosis due to surgery or radiation + Arm lymphedema : after axillary lymph node dissection after mastectomy
+ Lymphedema pelvic : after postoperative pelvic lymph node dissection (eg, urothelial carcinoma)
+ Neck lymphedema
Tumor: breast cancer, cervical cancer, Hodgkin lymphoma, melanoma, prostate cancer, metastasis. Lymphatic vessels: Femoral artery bypass surgery, trauma, radiation-induced fibrosis, infiltrative neoplasms, rheumatoid arthritis, filariasis, elephantiasis nostras verrucosa, recurrent infections (eg, tissue inflammation) cellulitis, vasculitis, trichophytosis)
5. Photographic characteristics
In the advanced chronic stage, the diagnosis is often a simple clinical diagnosis. Imaging is used to confirm the diagnosis, plan surgery, and during surgery. With early or intermittent disease, diagnosis can be difficult.
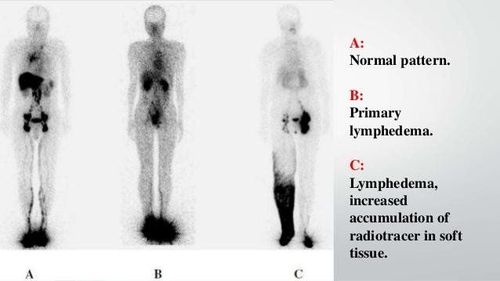
5.1. Lymphoscintigraphy Lymphoscintigraphy is commonly used to confirm the diagnosis of lymphedema and is a reliable method for evaluating lymphatic system function. It provides images of major lymphatic trunks and lymph nodes as well as an assessment of lymphatic function.
The colloidal radioisotope 99mTc-sulfur is injected into the intertoedial space of the affected leg, both intradermally and subcutaneously. Using stress tests, it is possible to determine the rate at which traces disappear from the injection site and its accumulation in the lymph nodes. Typical abnormalities in lymphedema include:
dermal back-flow Lost or delayed radioisotope transport Bidirectional filling with reverse flow Radioisotope in lymph nodes lost or slow
5.2. Magnetic resonance lymphography Magnetic resonance lymphography requires the acquisition of high-resolution 3D datasets of the entire limb. It is particularly useful for preoperative planning of lymphangiectasia, as it can show individual lymph channels and areas of retrograde flow to the skin. Two-pulse lymphatic magnetic resonance: + 3D heavily T2-weighted : showing the severity and distribution of lymphedema
+ High-resolution fat-suppressed 3D spoiled gradient echo (SPGR) after intravenous injection Intradermal contrast: description of lymphatic channels
+ MR venogram (also high-resolution 3D SPGR) can also be obtained after intravenous contrast injection to help distinguish superficial veins from lymphatic channels.
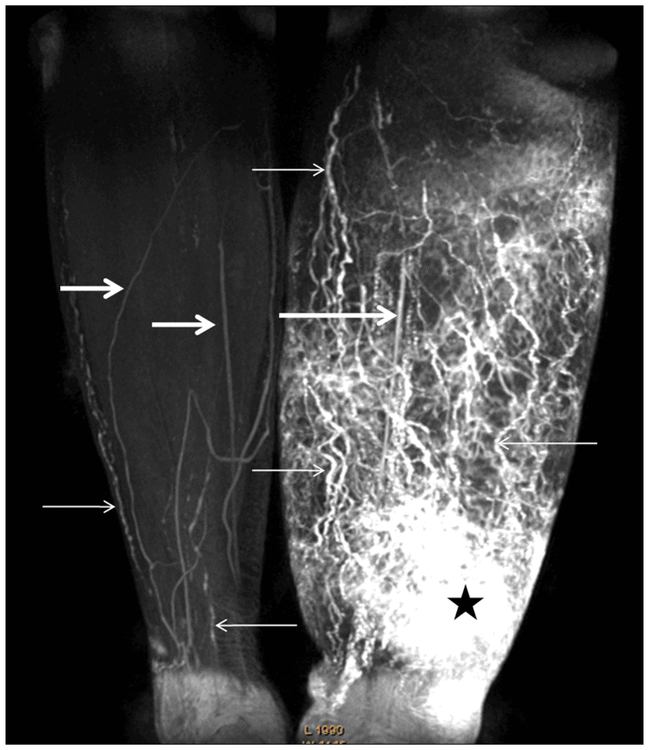
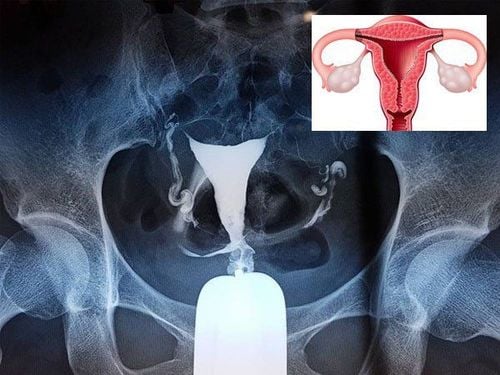
Figure 4:
3D Magnetic Resonance (MR Lymphography) with contrast injection in the lower leg. MIP image obtained 20 min after contrast injection of a 57-year-old woman with stage III left leg lymphedema and a history of radical hysterectomy following adjuvant radiotherapy.
Right leg normal, normal lymphatic vessels as a discontinuous line, with opacities (thin arrows).
Image shows multiple dilated rosary-shaped lymph vessels in the left leg (small arrows).
The dermal back-flow image is an irregular patchy hyperintensity area with a faint border above the left ankle (star).
Also visualized enhancing veins are linear structures of lower signal intensity (thick arrows).
5.3. Indocyanine green lymphangiography Indocyanine green lymphangiography is an emerging technique. It is comparable to MR lymphangiography in terms of sensitivity and specificity in the diagnosis of lymphedema and is superior to traditional lymphatic scintigraphy.

Figure 5. Illustration of lymphatic staining with Indocyanine green taken before liposuction; B: The green lymphatic line that appears on exposure is re-marked on the skin. Liposuction is not performed within 2cm around the red circle.
5.4. CT Scanner CT can be used to locate edema: subfascicular or suprafascial, and can show the characteristic honeycomb image of subcutaneous edema and thickening of the skin. However, its role in tracking is diminishing due to its inherent ionizing radiation.
6. Treatment
Lymphedema cannot be cured. Treatment focuses on reducing swelling and controlling pain. Treatments for lymphedema include:
Remedial exercises Arm or leg wraps Compressed air massage Compression clothing Complete decongestive therapy In severe lymphedema, your doctor Surgery to remove excess tissue from an arm or leg may be considered to reduce swelling. There are also newer techniques such as lymphatic-venous anastomosis or lymph node transplantation.
Vinmec International General Hospital is one of the hospitals that not only ensures professional quality with a team of leading medical doctors, a system of modern equipment and technology. The hospital provides comprehensive and professional medical examination, consultation and treatment services, with a civilized, polite, safe and sterile medical examination and treatment space.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.