This is an automatically translated article.
Posted by Doctor Mai Vien Phuong - Department of Examination & Internal Medicine - Vinmec Central Park International Hospital
Diabetic and postoperative gastroparesis are common physical disorders. Most patients with gastroparesis with no identifiable cause are considered idiopathic. This article will help learn about the association between neuromuscular disease and idiopathic gastroparesis.
1. Post-infectious gastroparesis hypothesis
Post-infectious gastroparesis has been reported in both children and adults, this condition being associated with various pathogens. The pathophysiology of postinfectious gastroparesis may be neurologic or muscular. The proposed mechanism is thought to be inflammation (an immune-mediated phenomenon, an exacerbation or manifestation of an underlying movement disorder). It is also documented that gastroparesis can occur due to viral damage.
In the pediatric literature, reports have linked rotavirus to idiopathic gastroparesis. Case series reported that among children with rotavirus-positive posterior gastroparesis, all fully recovered to gastric emptying in 6-24 months.
In an outbreak of 1300 subjects with domestic Giardia lamblia infection, 139 continued to have abdominal symptoms after initial infection. In this group, 22 patients with a negative follow-up stool analysis for Giardia were compared with 19 controls using gastric emptying. There was a significant delay in gastric emptying in subjects with prior Giardiasis infection, p < 0.01.
The esophagus, small intestine, and colon are commonly affected in patients with systemic sclerosis. Approximately 47-66% of patients with systemic sclerosis have delayed gastric emptying to solids. Dyspeptic symptoms such as nausea, vomiting, and epigastric discomfort are common in patients with systemic sclerosis. Delayed gastric emptying with fluid was detected by ultrasound in 20 systemic sclerosis patients compared with 20 healthy controls. It is hypothesized that collagen replacement by gastric smooth muscle may lead to subsequent decreased gastric motility in patients with systemic sclerosis.
2. Idiopathic gastroparesis and neuromuscular disease
2.1 Demyelinating disease Acute demyelinating disease is a rare cause of gastroparesis. This pathology can be suspected when the symptoms of gastroparesis are related to neurological impairment.
Antibodies against aquaporin water channel protein (AQP)-4 can cause a wide range of inflammatory, demyelinating, central nervous system disorders known as neuromuscular spectrum disorders (NMOSDs). Symptoms similar to gastroparesis include nausea, vomiting, and intractable hiccups. However, AQP4-IgG-positive patients did not demonstrate delayed gastric emptying.
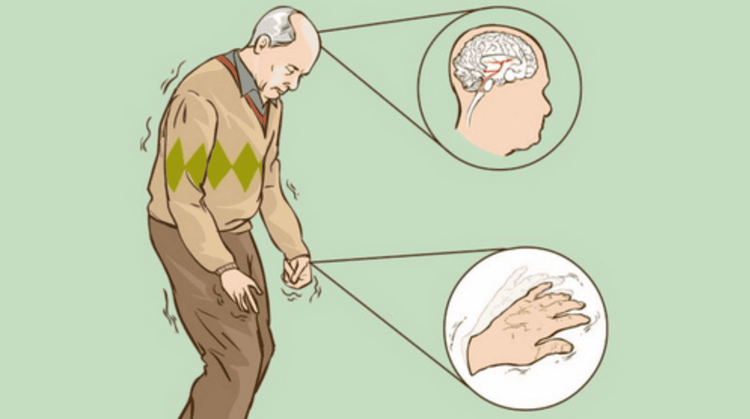
Multiple Sclerosis (MS): A demyelinating disease that damages the brain and spinal cord. The most common gastrointestinal complaints reported in MS patients are diarrhea, constipation, and dysphagia. Paraneoplastic syndromes: Paraneoplastic syndromes may present as esophageal dysfunction (pseudoachalasia), gastroparesis, pseudo-obstruction, or constipation. 2.2 Central Neurodegenerative Disease Patients with Parkinson's disease (PD) have been reported to exhibit delayed gastric emptying into solids. In a randomized study, 80 patients with untreated PD were compared with 40 healthy patients for solid or liquid gastric emptying. A total of 88% of PD patients had delayed gastric emptying with solids and 38% with liquids.
Abnormal gastric electromyography in untreated Parkinson's disease may be responsible for delayed gastric emptying. Lewy bodies have also been identified in the smooth muscle and intestinal neurons of Parkinson's patients.
2.3 Functional Gastrointestinal Disorders Approximately 40% of patients diagnosed with functional dyspepsia (FD) have delayed gastric emptying as the explanation for their symptoms. Patients with idiopathic gastroparesis are more likely to have frequent nausea and vomiting, while FD patients have postprandial asthenic syndrome, manifested by early satiety and abdominal discomfort. A meta-analysis of 17 studies found delayed gastric emptying with a relative risk of 1.46 (CI 1.23-1.69).
2.4 Gastroesophageal Reflux Delayed gastric emptying has been reported in 28 to 56% of patients with gastroesophageal reflux disease (RD gastric emptying). Theoretically, delayed gastric emptying would cause abdominal distention, increase the frequency of transient lower esophageal sphincter relaxation, and increase gastric emptying RD.
2.5 Visceral plexus ganglia compression or trauma Compression or trauma to the splanchnic plexus ganglia can interfere with parasympathetic signaling to the stomach, resulting in a loss of cardiac muscle coordination. Compression of the celiac axis by a fibrous band (median arch ligament) that connects to the diaphragm is called medial arch ligament syndrome (MALS), which is characterized by abdominal pain, nausea, and vomiting.
2.6 Hyperactivity syndrome Joint hypermobility syndrome (JHS) is a new addition to the association with GI symptoms. Patients with JHS have mobility of the joints, extensibility of the skin, and ease of brushing. In a controlled study of 336 patients with functional gastrointestinal disorders (FGID), 39% were also diagnosed with JHS. More specifically, 51% of FGID patients whose symptoms were mainly postprandial pain were diagnosed with JHS. Orthopedic orthopedic tachycardia syndrome (POTS), caused by a dysfunctional autonomic control mechanism, is associated with JHS in 60% of patients.
In a large cohort study of 163 POTS patients, 34% were normal, 18% had growth retardation, and 48% had rapid gastric emptying. In patients with JHS, autonomic dysfunction and decreased compliance of the intestinal wall may affect gastric emptying. The literature review showed that gastric tachycardia was more common in JHS patients with POTS. In the absence of POTS, the occurrence of rapid and slow gastric emptying is similar.
3. Other causes of delayed gastric emptying
Cystic fibrosis (CF): May be associated with GI dysfunction including gastroparesis, RD gastric emptying, and chronic constipation. The median life expectancy of CF patients living to adulthood is 37 years. In a systemic review, patients with CF had a high frequency of gastroparesis (38%) and this was more common in patients over 18 years of age. The coexistence of gastroparesis and CF can present significant nutritional challenges. Cases of gastroparesis in patients receiving radiation therapy to the abdomen, pelvis, and whole spine have also been reported: There are also GP reports of patients receiving high-dose chemotherapy and cell transplantation. origin. Treatment following gastroparesis chemotherapy is a rare occurrence and the pathophysiology behind this process is poorly defined. However, may be partially related to paraneoplastic syndromes or chemotherapy-induced neuropathy. Currently, Vinmec International General Hospital is a prestigious address trusted by many patients in performing diagnostic techniques for digestive diseases, diseases that cause chronic diarrhea or Crohn's disease...Especially , the screening techniques for gastric cancer and gastric polyps at Vinmec were performed using the Olympus CV 190 endoscope, the NBI function (Narrow Banding Imaging - endoscopy with narrow light frequency band) results in stool images. mucosal pathology is clearer... Thanks to that, the doctor can make an accurate diagnosis and give a timely treatment plan. Not only has a modern equipment system, Vinmec is also a place to gather a team of experienced doctors and nurses, especially, with a space designed according to 5-star hotel standards, Vinmec is guaranteed to bring bring the patient comfort, friendliness, peace of mind.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
References
Danny j. avalos, et al. Understanding the etiology and spectrum of idiopathic gastroparesis. Gastrointestinal motility and functional bowel disorders, series
22. april 2017 • volume xli, issue 4














